Post mortems reveal clear differences in the brain cells of people with depression
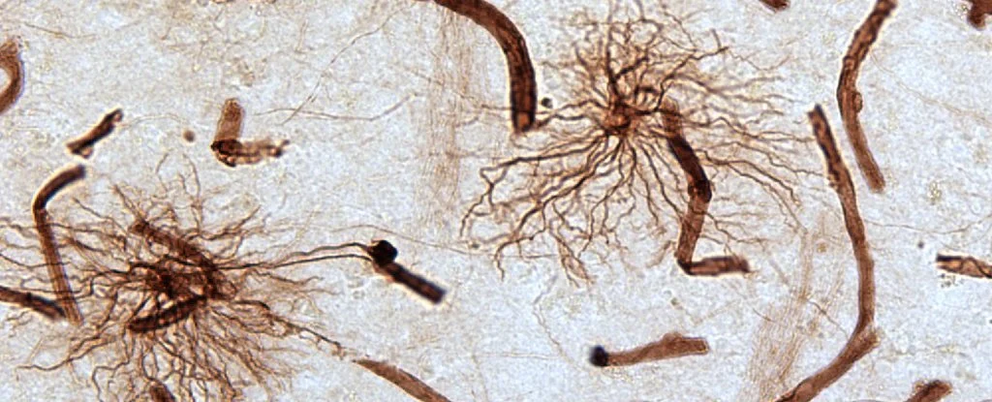
Stained astrocytes connecting to blood cells
A comparison of brain tissues taken from individuals who died by suicide has for the first time linked chronic depression with a stark drop in the number of specific kinds of supportive nerve cells.
While the finding doesn't demonstrate a cause for the decline, or necessarily describe how higher numbers of cells might protect mental health – if at all – it does establish a new area of investigation that could one day lead to early diagnosis and treatment for depression.
Researchers from Douglas Mental Health University Institute and McGill University in Canada analysed brain tissue taken from 10 men diagnosed with depression who passed away from suicide. These were compared with 10 samples of tissue taken by post-mortem from different brain regions in men who died suddenly without a mental-health diagnosis.
Of particular interest was the number of neural 'nanny' cells called astrocytes, a type of support cell.
Earlier investigations into potential differences in brain anatomy between those with chronic depression and those without have strongly hinted at a role for the brain's network of supporting cells, particularly in areas such as the prefrontal cortex and amygdala.
Such helper tissues play an important role in shuttling around nutrients, keeping charged molecules in balance, and healing trauma to the brain and spinal cord.
Depression is characterised by a wide variety of symptoms and behaviours, including a reduction or absence of pleasure and enjoyment, ongoing sense of guilt or grief, loss of appetite, and, in some cases, intentions of self-harm.
Exactly how these traits might emerge from changes in cells that simply lend our neural pathways a helping-hand is the big question.
Interestingly, it's come to light in recent years that astrocytes could be more hands-on with the communications side of nerves firing, making them not just nannies but potential traffic wardens with a far more dynamic responsibility.
Working out how these diverse astrocyte functions might be tied in with symptoms of depression requires investigating their structures and biochemistry, which isn't the easiest thing to do inside a living brain.
Researchers have made some headway in the past, finding a protein common to a number of cells in mammals – called glial fibrillary acidic protein (or GFAP) – isn't expressed in as high quantities by astrocytes in brains diagnosed with depression.
This is useful to know, but astrocytes that produce GFAP represent a minority of the overall population. So investigators are searching for ways to identify and compare other astrocyte features.
Vimentin is yet another kind of protein expressed by human cells, commonly used to give structure to certain cells. It's been linked with brain pathology in the past as well, making it a worthwhile target to study in the context of mental health.
"We analysed the astrocytes in the brain by staining specific proteins found in their structure - vimentin and GFAP," says neuroscientist Liam O'Leary, who completed this study while at McGill University.
"Vimentin staining has not been used before in this context, but it provides a clear, complete and unprecedented view of the entire microscopic structure of these cells."
The comparisons between different kinds of astrocyte were telling. Like the GFAP cells, vimentin-expressing astrocytes were significantly fewer among the samples of brain tissue taken from men with depression.
But the differences between the two in the prefrontal cortex were twice as great for the vimentin cells, strongly implicating a role for this particular flavour of support cell.
The findings form just a small piece of the puzzle behind chronic major depression. We're a long way off building a comprehensive model that connects discrete cell types with declines in mood and pleasure.
It's even likely that as we learn more, it'll become clear that a multitude of cell types, pathways, and structures can give rise to what is today one of the leading causes of disability worldwide.
But for those with the condition, knowing researchers are inching forward in understanding the physical basis of their mental health provides hope of better diagnosis, more effective treatments, or possibly even recovery.
"The promising news is that unlike neurons, the adult human brain continually produces many new astrocytes," says senior author and McGill University psychiatrist, Naguib Mechawar.
"Finding ways that strengthen these natural brain functions may improve symptoms in depressed individuals."
This research was published in Frontiers in Psychiatry.
If this story has raised concerns or you need to talk to someone, here's a list where you may be able to find a crisis hotline in your country.