What is prediabetes?
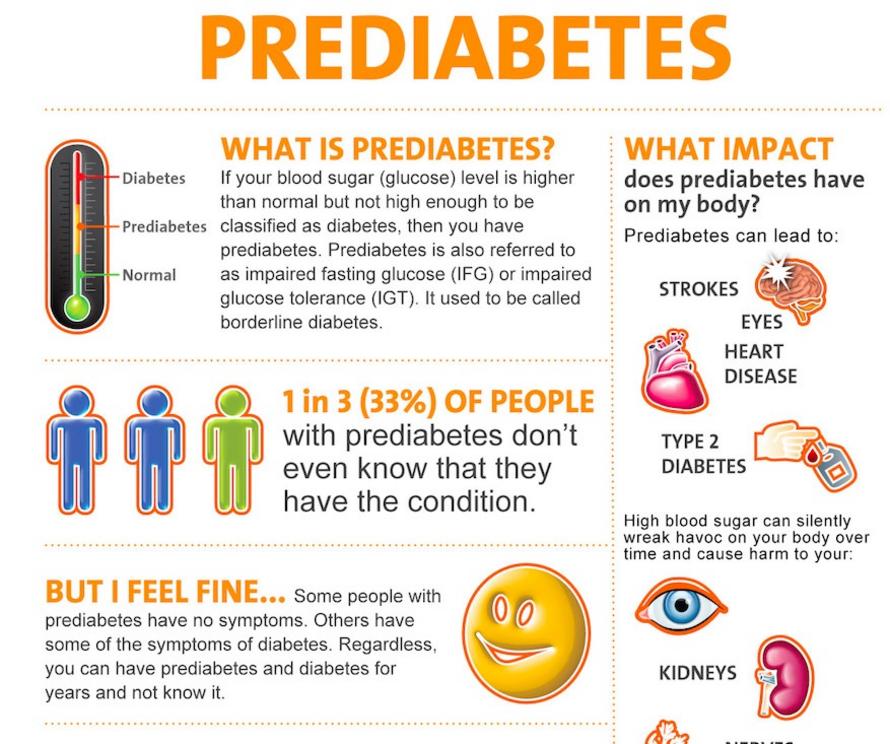
- Prediabetes is characterized by a slight elevation in blood glucose. An estimated 84 million American adults — about 1 in 3 — are prediabetic, and most are unaware of this fact
- Research by the late Dr. Joseph Kraft suggests a vast majority of people are diabetic even though their fasting glucose is normal. Only 20 percent of patients had a pattern signaling healthy post-prandial insulin sensitivity and low diabetes risk, which means 80 percent were prediabetic or had “diabetes in situ”
- Any meal high in grain and sugar carbs typically generates a rapid rise in blood glucose. To compensate, your pancreas secretes insulin into your bloodstream, which lowers your blood sugar
- Over time your body becomes desensitized to insulin, requiring more and more of it to get the job done. Eventually, you become insulin resistant and prone to weight gain, and then full-blown diabetic
- Researchers now believe there are at least five broad manifestations of diabetes: Type 1 or insulin-dependent diabetes, plus four different kinds of Type 2 diabetes
Insulin is absolutely essential to staying alive; unfortunately, the vast majority of people have resistance to this essential hormone, speeding up the aging process and contributing to the development of degenerative diseases. Any meal high in grain and sugar carbs typically generates a rapid rise in blood glucose. To compensate, your pancreas secretes insulin into your bloodstream, which lowers your blood sugar to keep you from dying.
Insulin, however, is also very efficient at lowering blood sugar by turning it into fat. The more you secrete, the fatter you become. If you consistently consume a high-sugar, high-grain diet, your blood glucose level will be correspondingly high and over time your body becomes desensitized to insulin, requiring more and more of it to get the job done. Eventually, you become insulin resistant and prone to weight gain, and then full-blown diabetic.
Majority of Americans Are Likely Prediabetic
Prediabetes1 is defined as an elevation in blood glucose over 100 milligrams per deciliter (mg/dl) but lower than 125 mg/dl, at which point it formally becomes Type 2 diabetes. According to the U.S. Centers for Disease Control and Prevention, an estimated 84 million American adults — about 1 in 3 — are prediabetic, and most are unaware of this fact.
However, this is a semantic moot point as any fasting blood sugar regularly over 90 in my book suggests insulin resistance. As you will read below, the seminal work of the late Dr. Joseph Kraft, author of “Diabetes Epidemic and You: Should Everyone Be Tested?” suggests that 80 percent — 8 out of 10 — of Americans are insulin resistant.
Based on data from 14,000 patients,2 Kraft, former chairman of the department of clinical pathology and nuclear medicine at St. Joseph’s Hospital, Chicago, developed a powerful predictive test for diabetes.3 He would have the patient drink 75 grams of glucose and then measure their insulin response over time, at half-hour intervals for up to five hours.
Interestingly, he noticed five distinctive patterns suggesting a vast majority of people were already diabetic, even though their fasting glucose was normal. Only 20 percent of patients had a pattern signaling healthy post-prandial insulin sensitivity and low diabetes risk, which means 80 percent were prediabetic or had “diabetes in situ.” As explained by IDMProgram.com:4
“If you simply wait until blood glucose is elevated, then you have [Type 2 diabetes], no question. But if you have normal blood sugars, then you may still be at risk of diabetes (prediabetes). So, we give a big load of glucose and see if the body is able to handle it … If the body responds by very high secretion of insulin, this will force the blood glucose into the cell and keep the blood glucose normal.
But this is not normal. It’s like the trained athlete who can easily run 10K in one hour and the untrained athlete who must dig deep and use all his effort to do so. Those people who need to produce prodigious amounts of insulin to force the glucose back to normal are at high risk [for diabetes].”
Four Kinds of Type 2 Diabetes
A team of Scandinavian researchers now argue that there are at least five broad manifestations of diabetes: Type 1 or insulin-dependent diabetes, plus four different kinds of Type 2 diabetes.5,6,7,8 To reach this conclusion, the researchers analyzed medical records of about 15,000 diabetic patients in Sweden and Finland. By looking at six common variables, including age of diagnosis, body mass index and severity of insulin resistance, the group found patients fell into five distinct groupings:
- Type 1: Severe autoimmune diabetes (SAID). Mostly young and otherwise healthy individuals with permanent insulin-deficiency due to autoimmune dysfunction.
- Type 2, subgroup 1: Severe insulin-deficient diabetes (SIDD). Young, typically healthy individuals with severely impaired insulin production. Includes those with high HbA1C, impaired insulin secretion and moderate insulin resistance.
- Type 2, subgroup 2: Severe insulin-resistant diabetes (SIRD). Overweight or obese patients whose bodies are still producing insulin but are no longer responding to it. Most of these have severely dysfunctional metabolism and display the most severe symptoms, including kidney damage.
- Type 2, subgroup 3: Mild obesity-related diabetes (MOD). Overweight and obese individuals who, while not insulin resistant, display mild symptoms. Most develop illness at a relatively young age.
- Type 2, subgroup 4: Mild age-related diabetes (MARD). Individuals who develop diabetes late in life and have mild symptoms.
According to lead author Leif Groop, an endocrinologist at Lund University Diabetes Center in Sweden and Folkhalsan Research Centre in Finland,9 “Current diagnostics and classification of diabetes are insufficient and unable to predict future complications or choice of treatment. This is the first step toward personalized treatment of diabetes.”
I personally believe these subtypes of Type 2 diabetes offer nothing but meaningless confusion. Kraft made it crystal clear: If you have insulin resistance — remember that is 80 percent of the U.S. population — you either have outright Type 2 diabetes or prediabetes, period. Fortunately this is one of the easiest problems in health to correct. All one needs to do is follow a cyclical ketogenic diet as I outline in my book “Fat for Fuel.”
Controversy Over Diabetes Guidelines
The following blood tests will help you determine whether you might be prediabetic or diabetic:
- Fasting glucose test. Generally speaking, a fasting glucose level below 100 milligrams per deciliter (mg/dl) suggests you're not insulin resistant, while a level between 100 and 125 mg/dl is suggestive of prediabetes, which means you’re mildly insulin resistant.
- Hemoglobin A1C test, which measures the average glucose in your blood over time, is done two to four times a year. This is a better test than a fasting glucose. An A1C level between 5.7 and 6.4 is considered prediabetic. Anything over 6.5 is diagnosed as diabetes. The higher your level, the worse your insulin sensitivity is.
- Fasting blood insulin test. This is an even better test. A normal fasting blood insulin level is below 5, but ideally, you'll want to be below 3.
- Oral glucose insulin test. This is the best and most sensitive test. It’s done identically to the OGTT (oral glucose tolerance test) but it also measures your insulin level. You compile the data and review Kraft’s book to determine if you are prediabetic, which is FAR more accurate than fasting glucose or even insulin levels.
Not surprisingly, conventional medicine remains clueless and the American College of Physicians (ACP) is now arguing for even less aggressive blood sugar targets when treating Type 2 diabetes.10 According to ACP president Dr. Jack Ende, “There are harms associated with overzealous treatment or inappropriate treatment focused on A1C targets.” In a new set of guidelines, the ACP now recommends aiming for an A1C between 7 and 8 percent, rather than the lower levels recommended by many diabetes groups.
For those who have already achieved a lower level, the ACP suggests reducing or stopping medication altogether and “just allow the A1C to be between 7 and 8.” The American Diabetes Association has firmly rejected the ACP's recommendation, and considering the risks involved, it seems really unwise to “just allow” your level to remain as high as 8 without addressing it. The best way to tackle it, however, is not with medication but with lifestyle changes.
Most Type 2 Diabetes Cases Are Completely Reversible Without Drugs
 pinterest.com
pinterest.com
It’s important to realize that Type 2 diabetes and prediabetes are rooted in insulin (and leptin) resistance, and that a vast majority of people — likely around 80 percent — are affected. This means it’s a rare individual who does not need to address his or her diet and physical activity, as these are the two most important and most effective prevention and treatment strategies. The good news is Type 2 diabetes — regardless of the subtype — is fully preventable and reversible without drugs.
I originally wrote my book “Fat for Fuel” for cancer patients, but it is even more effective for Type 2 diabetes. Cancer is a complex and typically a major challenge to treat, requiring more than diet. However, Type 2 diabetes in nearly every case is resolved with the type of eating plan I discuss in “Fat for Fuel.”
So, remember, if you’re at all concerned about your health, addressing any indication of insulin resistance and prediabetes is really crucial. Here is a quick summary of some of the most important guidelines. Taken together, this plan will lower your risk of diabetes and related chronic diseases and help you to avoid becoming victim to a health condition you might not even realize you have.
Limit added sugars to a maximum of 25 grams per day. If you're insulin resistant or diabetic, reduce your total sugar intake to 15 grams per day until your insulin/leptin resistance has resolved (then it can be increased to 25 grams) and start intermittent fasting as soon as possible.
Limit net carbs (total carbohydrates minus fiber) and protein and replace them with higher amounts of high-quality healthy fats such as seeds, nuts, raw grass-fed butter, olives, avocado, coconut oil, organic pastured eggs and animal fats, including animal-based omega-3s. Avoid all processed foods, including processed meats. For a list of foods that are particularly beneficial for diabetics, please see “Nine Superfoods for Diabetics.”
Get regular exercise each week and increase physical movement throughout waking hours, with the goal of sitting down less than three hours a day.
Get sufficient sleep. Most need right around eight hours of sleep per night. This will help normalize your hormonal system. Research has shown sleep deprivation can have a significant bearing on your insulin sensitivity.
Optimize your vitamin D level, ideally through sensible sun exposure. If using oral vitamin D3 supplementation, be sure to increase your intake of magnesium and vitamin K2 as well, as these nutrients work in tandem.
Optimize your gut health by regularly eating fermented foods and/or taking a high-quality probiotic supplement.
For full references please use source link below.

