The Age of Polio Revisited
Dan Olmsted wrote, But the question remains, and it remains important, because while the worldwide eradication effort makes slow progress, related viruses like EV-68 -- which paralyzed and killed children in the U.S. -- are surfacing, and other diseases with similar characteristics are waiting for their moment."
All 8 parts of Dan's series are below. He was planning to write a book on The Age of Polio, an epidemic he believed was a result of environmental toxins triggering the virus. I miss Dan every day. How we could have benefited from his writing today. Kim
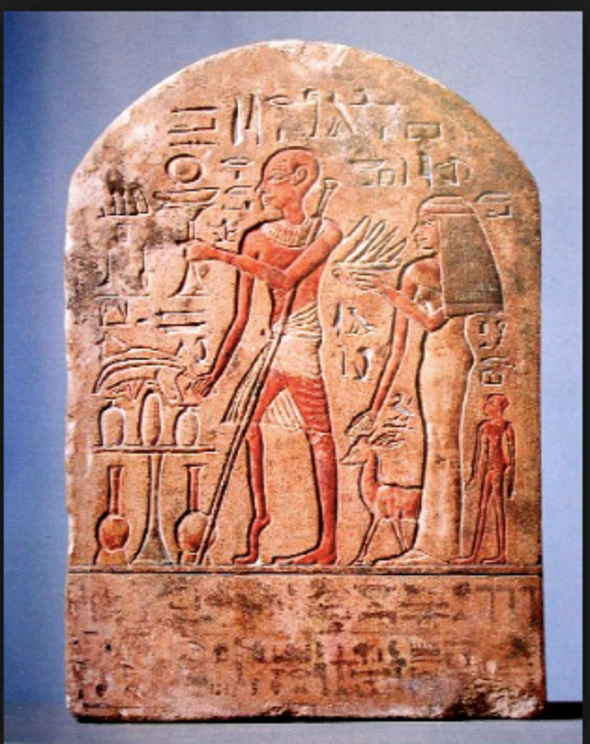
Limestone stele of priest with withered leg. Fourteenth Century BC by anonymous stonecutter.
By Dan Olmsted
"Everything should be made as simple as possible, but not simpler." -- Albert Einstein
1.
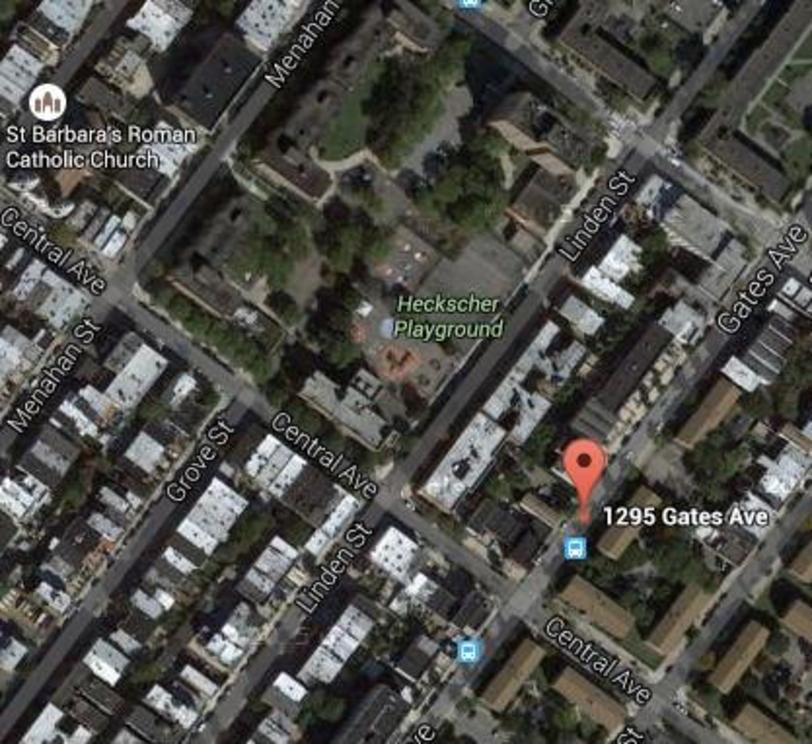
On May 1, 1916, thirteen-month-old Lettie Caruso* moved with her family to a tenement at 1295 Gates Avenue, Brooklyn. A fifty-six-year-old woman named Mrs. G.H. Franklin lived and worked on the first floor, where she ran a small ice cream parlor that “the children naturally frequented,” according to a subsequent report by the New York Health Department. Lettie and her family lived in the apartment adjacent to the ice cream shop. On May 9, Lettie became ill. “A private physician was called the first day and came several days,” the Department reported. “She was examined with the stethoscope and at the first visit the doctor thought it was only a cold. As she grew worse a physician from New York was called in consultation. Mrs. Caruso thought the diagnosis was pulmonary bronchitis. So far as she knew the child was not paralyzed, but she cannot remember any special examination for that. There has been no Infantile Paralysis in this house, nor in the adjoining properties.”
That was about to change.
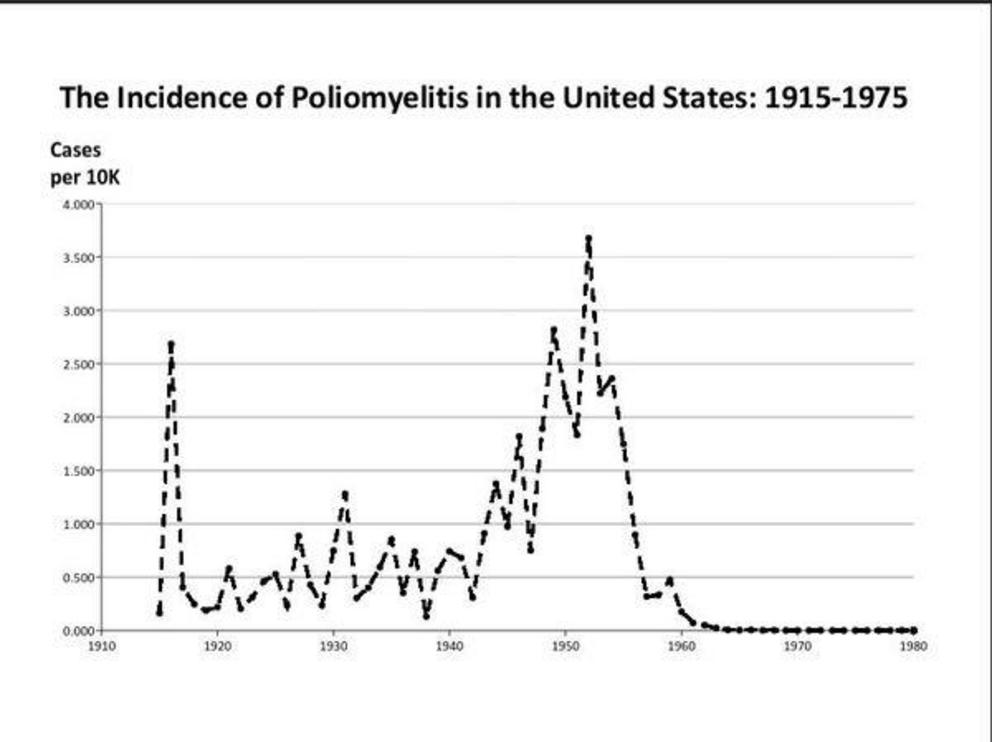
Looking back with perfect hindsight, Brooklyn in May 1916 was ground zero for an explosion that no one saw or heard for a month and more -- and, to this day, no one has satisfactorily explained. Before it ended late that summer, 25,000 people in the Northeast developed paralytic poliomyelitis, most of them young children, and an extraordinary 5,000 died -- nearly half of them in the City of New York, a toll approaching the September 11 tragedy. It was by far the largest and most lethal polio epidemic to date, and it remains one of the biggest ever (see chart).
As spring turned to summer, polio gripped every parent with fear, not just in the Northeast but nationwide. It was a fear that never entirely lifted until the outbreaks ended in the U.S. and most other countries after the Salk vaccine was introduced a half-century later, an occasion so momentous that church bells rang out across the country. But 100 years ago, and especially Brooklyn, there was barely suppressed panic that the authorities and the media did their best to tamp down.
"While there is no need of undue alarm," the Brooklyn Daily Eagle reported in a careful front-page (but one column) article on June 17 announcing the epidemic, "the officials of the board of health are somewhat worried and are taking measures to stamp out the disease."
Since 1894 there had been smallish though increasingly ominous clusters of cases around the country. The first, in Vermont, affected 132 and killed 18; strangely, domestic animals were also affected even though polio is a disease of humans. The worst so far had been in 1907, which began in Brooklyn, too, before spreading to Greater New York but not much further, killing 125 in the city. Around the world, particularly in Scandinavia, larger clusters had started appearing, seemingly at random, since 1905.
But 1916 marked the moment the Age of Polio arrived in America.
Perhaps because the outbreak rose and fell so suddenly, bracketed by much that came to define the turbulent 20th century -- war in Europe in 1914, the sinking of the Lusitania, which departed from New York Harbor the next year; shark attacks along the crowded Jersey shore that sweltering summer of 1916 that caused sensational press coverage and became fodder for Jaws 60 years later; U.S. entry into WW I in 1917; and the Influenza Pandemic that killed 2,157 New York City residents in the week of November 1, 1918, alone -- the epidemic has faded from collective memory.
But the question remains, and it remains important, because while the worldwide eradication effort makes slow progress, related viruses like EV-68 -- which paralyzed and killed children in the U.S. -- are surfacing, and other diseases with similar characteristics are waiting for their moment. So this series asks: What set off the Explosion of 1916? Why didn't it spread like that again till after World War II? This work picks picks up on reporting Mark Blaxill and I conducted over a number of years and first set out in our Age of Polio series in 2011. We decided to focus next on a single polio outbreak to see if we could find evidence for our hypothesis that epidemics resulted from an interaction of the virus with novel environmental toxins.
So this is a logical step -- from the global to the granular, from broad strokes to a concrete case study -- but also a risky one, because it can easily devolve into the dreaded “confirmation bias” and “availability cascade” where everything seems to point toward one’s own pre-conceived idea. I’m sure that if I looked hard enough I could connect rats with insects with milk with horse stables in just about every single polio case. All those possible routes, frantically scrutinized in 1916, now occupy orderly manila envelopes at the American Philosophical Society library in Philadelphia, where the New York Department of Health’s contact-tracing records have, fortunately, been preserved. (None appears to have played a significant role in polio outbreaks.)
This report reflects our overall mission of looking for the hidden causes of modern illness. We believe those causes are not exclusively microbes -- the 20th century model -- but also environmental toxins about which mainstream science and medicine have been far too blasé and incurious. We need better models of what causes mysterious illnesses from autism to polio to schizophrenia. For all those and more, there is evidence for an environmental role. But because that role is usually missed or even suppressed, nothing is learned before the next contagion explodes onto the scene and medicine resorts once more to a war on the virus alone.
To understand modern illness, in short, we need to finally understand polio.
What set off the Explosion of 1916? If I'm right, an environmental bomb landing in just about the worst possible place at the worst possible time set it off, the impact spreading with a smooth but terrible precision like ripples from a pebble dropped into a still volcanic lake.
2.
On May 23, Lettie Caruso died. She was an only child.
The cause of death was listed as “fatal pneumonia.” Soon there was more sickness and death in the building. At some point in May, “there was a woman living on the top floor of the house over her [Mrs. Franklin's ice cream] store whose baby was taken ill and died suddenly. … The doctor was an Italian and never told the mother the cause of the baby’s death.” Based on another report in the file, this second infant was probably a male named Peter: “After an illness of 4 days, Peter Pinchero of 1295 Gates Ave. died on May 24th. Eight days before he was taken ill, his cousin, living at the same address, had also died following a similar illness of about two weeks.” (This is probably an imprecise reference to Lettie.)
Contact tracing, as it's called, was not an easy task, as the jumble of interviews and observations in Lettie's file attest a century later. Between the language barrier in this Italian neighborhood, the poverty, and especially the fear that health officials might take children away, the truth comes out in dribs and drabs and even then remains incomplete. Children get sick and die, their heartbroken and terrified families move away, someone remembers and someone else misremembers what happened when. Nor did the health workers exhibit much empathy, calling their clients "suspicious and ignorant." “These people neither understand not speak Eng. So I could get very little accurate information,” a nurse wrote August 24 as she tried to complete a questionnaire on “possible source of infection” at the tenement the previous May. (Apparently there were no Italian speakers in the employ of the City of New York to call on in the midst of the worst polio epidemic ever.)
Another typed note suggests two more Pinchero cousins and an aunt who lived in the tenement became ill during May, but recovered. Summing up: Three or four related Italian families were living in a tenement house in Brooklyn in May 1916. Two children died, two of their cousins and an aunt got sick but recovered. Exactly what they suffered from was unclear, though their names found their way into the health department's contact-tracing files as possible early sources of infection. If Lettie Caruso and her cousin had polio, they were among the handful of very early cases with onset that fateful May. Either way, their stories are telling us something.
--
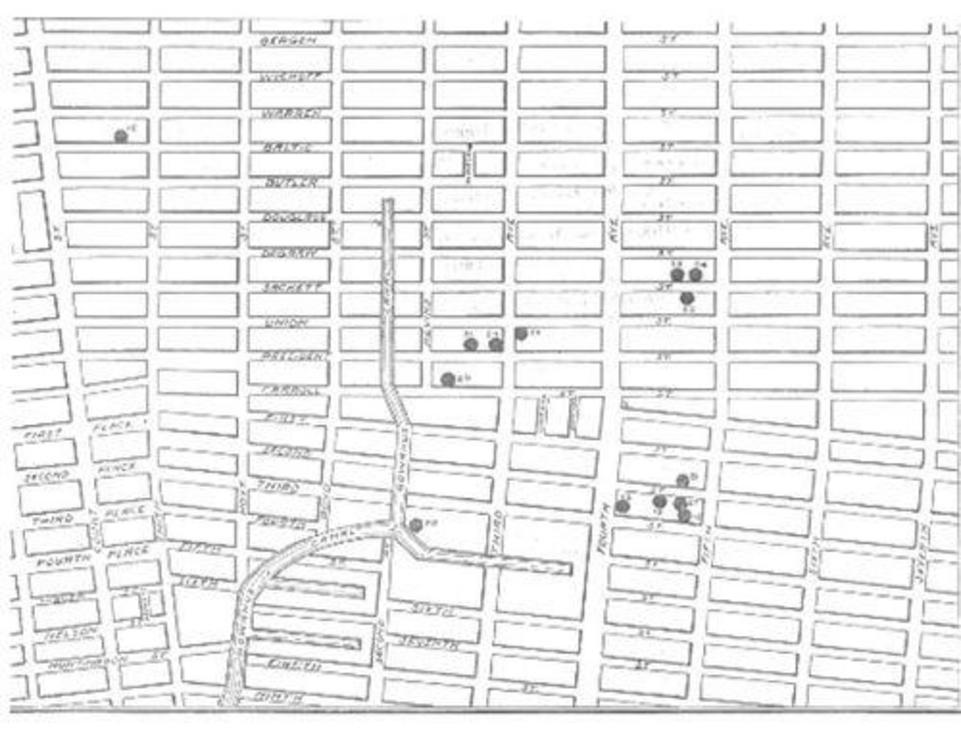
A near-simultaneous outbreak in an Italian neighborhood around the Gowanus Canal, about four miles west, became known as the epicenter of the epidemic. The neighborhood and its characteristics have been studied and speculated about ever since: Was the virus in the canal? Did it get into the drinking water supply? Did the Italians bring a new strain with them from Italy to which more children were susceptible? One recent speculation is that the Rockefeller Institute, which was conducting studies on the virus at its headquarter in Manhattan, somehow let the virus loose and it traveled a few subway stops to Brooklyn. In any event, half of the 24 cases of polio in Brooklyn that month clustered around the canal.
Today the area is hip, hot and happening, anchored by a Whole Foods nestled in the fork of the canal. A Superfund project aims to clean the whole area up, and former warehouses have been recast as pricey lofts. Hillary Clinton’s campaign headquarters is less than two miles away. Back in 1916, there was nothing organic about this neighborhood. It was not far from an area called Pig Town, named for the animals that were raised there by the immigrants, with a soupçon of general squalor implied. It was known for the filthy conditions brought on by poverty, poor municipal services and the general location at the edge of heavy industry that casually flung its garbage over its shoulder. Sewers overflowed, vacant neighborhood lots where kids played were overrun by garbage. The whole thing was barely above sea level -- most of the time.
According to a description from the Brooklyn Daily Eagle of May 9, 1885:
“The overflow from the pig wallows at the bottom of the other lots comes down through drains beneath the filled in streets. At high tide the water backs up through these drains as far as Huntington street. The furthest inland of the chain of ponds thus formed is only a block away from Public School No. 27, on Nelson street, near the corner of Columbia, at which 1,500 children attend. Within 100 yards of the public school is a vast public dumping ground, running westward for a long block, from Delevan street, between Dwight and Richards. A great deal of putrid and offensive matter lies on this dumping ground, mingled with the ashes which the contractors' men bring there. Among the worst of this decaying animal and vegetable matter may be classed refuse from the sugar refineries in the neighborhood.” (The “pig wallows” described above are to the left of the canal, and sustained many cases of polio.)
The fact that polio would break out in such an area might seem logical, because polio is a microbe that thrives in filth and is transmitted by feces; a land of overflowing sewers and industrial gunk where urchins roamed would seem the perfect place. But it’s counter to the now-orthodox belief that polio epidemics broke out around the turn of the 20th century because sanitation had finally improved. This is the crux of the so-called “hygiene hypothesis.” Under this widely accepted theory, children in less sanitary times used to be exposed to illnesses earlier, when they were still protected by temporary immunity passed on from their mother. The later you got a disease, the more that immunity had waned, and the worse it was, under this theory. In other words,” an authoritative account puts it, “epidemic poliomyelitis can be considered an unfortunate consequence of the invention of the flush toilet.” If the hygiene hypothesis is true (I don't buy it), this was the last place on earth from which you’d expect the worst polio epidemic in history to emerge.
This is just one of the facts about the rise of polio that simply don't fit the standard model. Albert Sabin, inventor of the live vaccine, mused in 1947: “No circumstance in the history of polio is so baffling as its change during the past fifty or sixty years from a sporadic to an epidemic disease.” In 2008, Neal Nathanson of the University of Pennsylvania School of Medicine wrote: "Surprisingly, there remain many important gaps in our understanding of the pathogenesis of poliomyelitis." Once the epidemic era ended in the developed world ended by the early 1960s, researchers put their attention elsewhere. That may have been an epic error.
--
Mrs. Franklin soldiered on in her storefront ice cream shop on Gates Avenue, though it’s easy to imagine that after two deaths and several illnesses an oppressive cloud hung over a place "all the children" frequented. “During this time she had kept the store open and had herself waited on the customers who came into the store,” the health department reported later. By the beginning of June she was beginning to feel ill, with pains in her neck, arms and legs. But like some sort of Calvinist Typhoid Mary, she just kept at it. On June 19, Mrs. Franklin was working at the store as usual when she suddenly fell unconscious to the floor. When she came to, she was paralyzed. She was taken to the hospital and began a long journey we will return to later.
What was going on here? Two children in the building had already died -- of what is uncertain -- and two more along with an aunt were sick but recovered. Now a 56-year-old woman -- way past the usual age -- had succumbed to something that looked a lot like polio. When all the statistics were recorded for the New York City epidemic, Mrs. Franklin's remained the oldest case on record.
3.
The small clusters of poliomyelitis cases in Brooklyn that May did not immediately catch the attention of the health department. It’s not that polio was unknown or unexpected: Since the turn of the century, epidemics hit the city with deadly regularity, though usually later in the summer. The one in 1907 killed 125 in New York City alone. This one would go on to kill twenty times as many -- 2,343 in the city and 6,000 nationwide.
The Brooklyn Daily Eagle story June 17 that reported “no need of undue alarm” also said "the officials of the board of health are somewhat worried and are taking measures to stamp out the disease," mostly centered on travel restrictions, quarantine, removal of sick children to hospitals, and sanitation efforts. In retrospect, Health Commissioner Dr. Haven Emerson wrote the next year: “To judge by the reports of physicians up to June 1, there was nothing to excite suspicion that we were already at the outset of an epidemic. Within the first eight days of June, 6 cases were reported from Brooklyn, from which borough no cases had been reported up to this time in 1916 and none in June from the other boroughs. The six cases were reported as follows”:
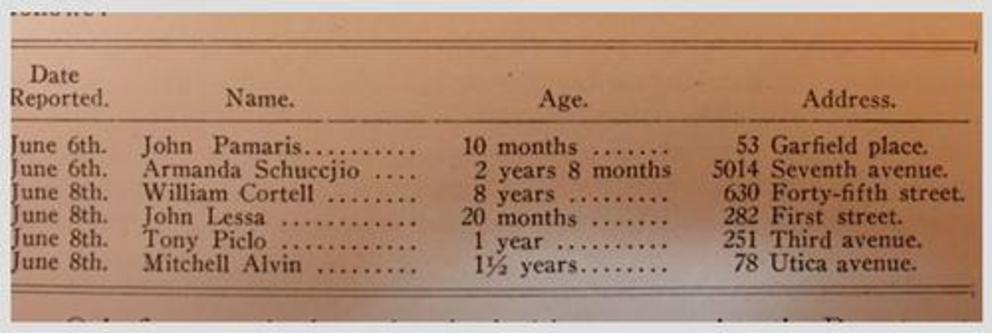
This list conveniently omitted the existence of the May cases. But even now, with names and neighborhood documented, it took another 10 days to raise the battle flag. Emerson claimed he had moved as fast as possible – given obstacles conveniently not of his creation. “Only a thoroughly alert public and a forewarned profession could have prevented the delay in official knowledge of the threatening epidemic,” he wrote in the department’s own exhaustive and self-serving 391-page history, "A Monograph on the Epidemic of Poliomyelitis (Infantile Paralysis) in New York City in 1916: Based on the Official Reports of the Bureaus of the Department of Health,” published in 1917, from which the above list is taken.
“That energetic measures were taken as soon as six verified cases of the disease were reported on June 6th and 8th, is a sufficient reply to any lingering suspicions that the Department of Health awaited the actual presence of a calamity before taking measures of protection.” That sounds like a guilty conscience that needed no accuser, but might have encountered a few. It also raised the question: Just whose responsibility was it to alert the public and forewarn the doctors about an annual epidemic that visited New York with increasing virulence?
But help, perhaps too much and too late, was on the way.
“On July 6,” Emerson writes, “the Secretary of the Treasury in person offered to the Mayor the assistance and cooperation of the United States Public Health Service. … The offer was gratefully accepted.” (I’ll bet it was.) That, said John R. Paul, whose 1971 “A History of Poliomyelitis” is considered the authoritative text, “posed a certain amount of competition for Dr. Emerson’s own working force.” (I’ll bet it did.)
Nonetheless, Paul wrote, Emerson displayed “earnest zeal” and “gave to this cause the very best that was in him – according to his lights.” But he and the Public Health Service zeroed in on quarantines and travel restrictions and studies of horse stables and side issues like documenting secondary exposures, which Paul called “a thankless task indeed.” (Those are the files at the American Philosophical Society in Philadelphia on which my reporting is based, so I do thank them for that! It's a researcher's dream.) A better focus would have been to collect information that “had to do with poliovirus – its distribution within the body and its distribution within nature,” Paul wrote. The fact that polio infection was caused by a "filterable virus" had only been established in 1908, after the last big epidemic, so a focus on it now would have been a significant contribution.
As for Emerson the man (below), “In appearance Haven Emerson’s tall, almost ascetic figure has epitomized the title which had been bestowed on him, namely, 'The last of the great Puritans.'" He was related to Ralph Waldo Emerson. But earnest zeal and rectitude did not always win the day. “After the lapse of fifty or more years it is easy to say what should have been done,” Paul wrote. “In retrospect, the tragedy was that, in view of the galaxy of talent which had been assembled on advisory committees and working forces alike and the administrational and laboratory facilities that were at their disposal, a golden opportunity to advance knowledge of the clinical virology of poliomyelitis had been allowed to slip by.” As regards Emerson’s own claim that the department’s response proved “the efficacy of co-operation,” Paul writes ruefully, “It cannot be said that these words have stood the test of time, though they may have been appropriate in 1916-17.”
Earlier notice might have stopped or at least foreshortened imminent threats like Mrs. Franklin working at her ice cream store on Gates Avenue for nearly three weeks after she started feeling pain in her arms, legs and spine on June 1. One has to think that being the friendly neighborhood ice cream lady for so many children so early in the epidemic, and “attempting to bathe” one of the children who subsequently died, and working until she literally dropped, was not a good idea. An earlier alert might have kept her at home or in the hospital, or scared patrons away, well before June 19, when she collapsed on the ice cream parlor floor. By the same measure, health officials didn’t notice or follow up on any number of anomalies -- deviations from the norm that often contain the best clues to causation, especially when they occur early on.
Mrs. Franklin herself was chief among them. Given that she worked with children all day -- including two who died in her building in the month of May -- it beggars belief she had remained unexposed (“non-immune” in public health-speak) to the common poliovirus for 56 years until one fine day in spring 1916. It makes you think about what she did for a living, which is both inevitable -- sell ice cream to children. If you want to look like a fool, mention ice cream and polio epidemics in the same sentence, as I just did. The two have entered folklore and science class as twin icons of false correlation – you might as well write "Stupid" on your forehead, backwards. Yes, it’s possible to show an amazing association between the two – because, as the statistically literate patiently explain, ice cream sales rose in the summer, and so did poliomyelitis cases, the former because it was summer, the latter because the virus appeared at that time of year. Just for fun, here’s one of those charts.
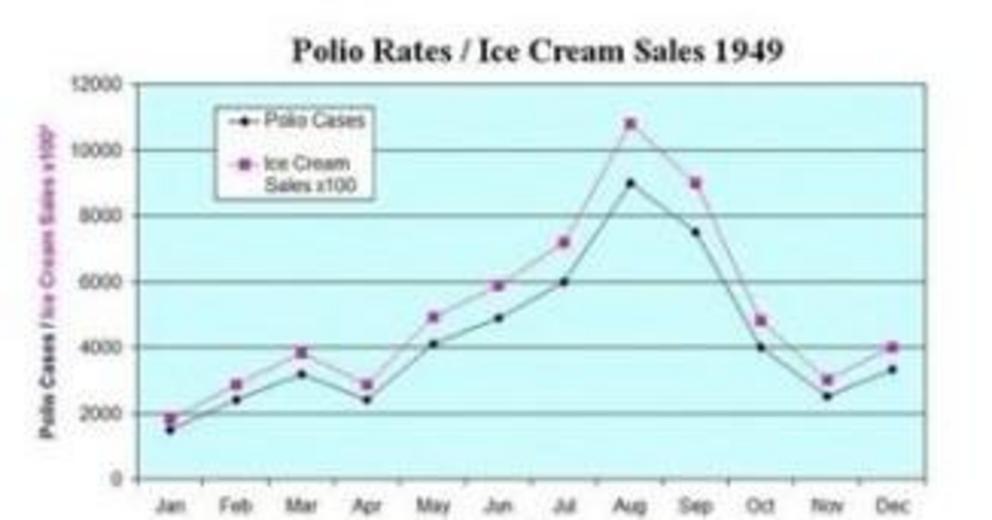
Similar charts can be concocted to associate ice cream sales with murder, shark attacks or the folly of your choice. (An article I wrote on another topic was once accused of this exact fallacy; I’ve been “ice-creamed.” I know the cold, drippy feeling.) But to persist in folly just a bit longer, where did the ridiculous idea of polio and ice cream come from? The ice cream hypothesis, as it has reached us today, appears to date from a 1948 effort to get the nation to cut out sweets, based on a doctor’s hypothesis that ice cream sales and polio cases were correlated because blood-sugar levels were supposedly related to polio risk. (The details don’t matter here, though one wonders if the doctor saw an association that might have been valid, then jumped to a conclusion that wasn't.) The doctor’s suggestions included: “1. Eliminate from the diet sugar and foods containing sugar, such as soft drinks, fruit juices (except tomato juice), ice cream, cakes, pastries, pies, candies, canned and preserved fruits. Saccharin may be substituted for sugar. Cut down the consumption of starchy foods, such as bread, rolls, pancakes, potatoes, rice, corn, cereals, grits.”
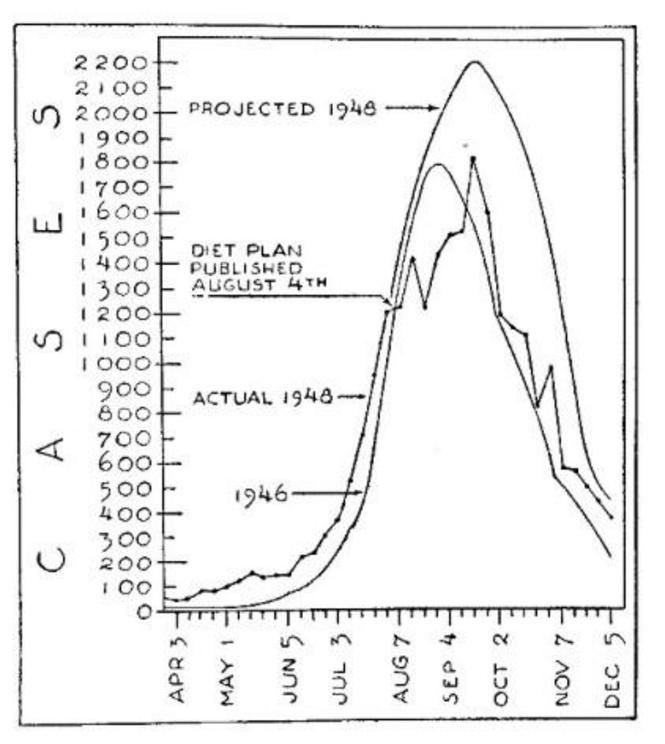
The diet drive was centered in North Carolina but became national news, and the polio rate did seem to dip a bit that year both there and nationwide, if you counted in a very particular way (see chart). You can read about it here. The chart essentially shows that while polio deaths were projected to reach 2,200 in 1948, they only hit 1,800, about the same as 1946, and slowed just as the diet plan was introduced.
The experts laughed. Less well known is that there was already concern about exactly those foods bearing some relationship to polio outbreaks, and it was quite prominent in the summer of 1918. First of all, the health department case files are replete with careful notations about what people ate and where they bought their fruit, vegetables, meat and milk -- it wasn't just kooks who were interested, it the was department itself. And a lot of people in New York City thought ice cream, cake, soda and other sweets and treats consumed by children in the summer especially, were involved. "In previous epidemics, the theory has been repeatedly advanced that food or drink may act as vehicles of infection in poliomyelitis," Dr. Emerson wrote in in the 1917 report. "The regular water supply and various foods and drink, particularly ice cream cones and soda water, have been under suspicion and investigation." I assume soda water means soft drinks.
Later in the monograph, he derided such speculation with a Puritan’s version of LMFAO! Dr. Emerson: “It may not add to the sum of scientific data to quote the suggestions received by the Department of Health as to the cause and means of curing or preventing poliomyelitis; but as a record of human interest the letters sent from all over this country and from many foreign lands present a picture which it is well for health officers to bear in mind. One hardly knows whether to laugh at the fantasies or weep over the ignorance and superstition exhibited.
“Two hundred and thirty suggestions as the cause of the disease were received, the largest number of authors (80) attributing the existing calamity to foods. Ice cream, soft drinks, candy and summer fruits were generally accused, cereals and canned foods coming second in favor.” Dr. Emerson, obviously, saw no basis for “attributing the existing calamity to foods.” So food and polio is a ridiculous connection, right, even though more than a third of 230 letter writers cited it? That's what Dr. Emerson just said. Well, hold that thought, because a few pages later he says this about the 1916 epidemic:
“There seems to be a well-marked tendency for cases in Manhattan to appear in the immediate vicinity of stables, groceries, meat or poultry markets, lunch rooms, delicatessen shops and bakeries or macaroni factories. … It is surprising with what regularity one or the other is found in the building next door to a house in which poliomyelitis has occurred. Others who have also examined the same districts with an unbiased mind, seem always to believe that cases range themselves with a definite relation to shops of this type. It has been repeatedly pointed out in earlier epidemics that stables are often associated with cases of poliomyelitis. This has been undoubtedly true in New York during the present summer, but the other association with provision shops has also forced itself upon our attention.”
So: in 1916 “unbiased” observers, and not just loony-toon letter writers, noticed "with regularity" and in fact "always" (just quoting the man here) a "definite relation" between cases of polio and places that served and sold food, especially certain kinds of food (along with that hoary old suspect, stables). Amazing! Even more amazing: On the facing page, the book includes a chart of associations between food and infection in “one of the somewhat better districts where there has been a group of scattered cases in the Bronx,” as well as a group from Manhattan.
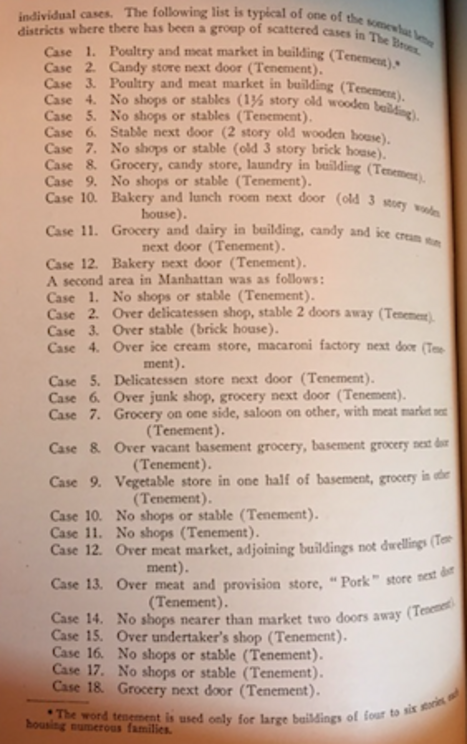
Here's what I take away:
Candy.
Grocery.
Bakery.
Ice cream.
Candy.
Grocery.
Bakery.
Ice cream.
Candy.
Grocery.
Delicatessen.
Grocery.
Lunch Room.
Grocery.
Doesn't that overlap with the list that Dr. Emerson was cackling about when he wrote, “Ice cream, soft drinks, candy and summer fruits were generally accused,” along with cereal and canned foods that you'd get at a deli, a grocery, a lunchroom? (And isn’t that just about the same list as the 1948 diet plan suggested cutting out -- "sugar and foods containing sugar, such as soft drinks, fruit juices (except tomato juice), ice cream, cakes, pastries, pies, candies, canned and preserved fruits"?) I vote yes. In his written discussion, Dr. Emerson puts stables first, the generic "grocery" second and meat markets third, and doesn't mention ice cream or candy at all, despite their equal or greater preponderance in the full-page list. Stables that attracted flies fit with his hypothesis; meat and grocery markets that attracted vermin did, too; ice cream didn't. But why not? If flies or rats or bad milk might spread the outbreak, why not the kinds of food cited both by the letter writers and the "unbiased minds"? Digging through a couple dozen folders in the health department archive of case reports, I found several more references. From my notes:
--
another case of child died, on july 26, father works in bakery rear apartment, a kitchen and bedroom which adjoin an ice cream shop in a filthy condition – also shop condition poor – selling ice cream and lemonade.
--
died age 4.5
used dipped milk from grocery. Unwrapped bread, apples that were peeled before given to child. Child would go to corner of street for horton’s ice cream in cones.
--
20 months old was taken sick august 1. … the grandfather bought ice cream for her on west end ave. near 66th st about two days before she was sick. They afterwards found there was a child in the family ill with poliomyelitis.
--
These, let’s remind ourselves before others do, are random anecdotes, the kind that lead to snickering about ice cream and polio charts. So let's be cautious. But these references in the first few files I examined, our of several thousand, make me think there must be more such reports, many of them from just the sort of people Dr. Emerson laughed off.
Let's look at another possible "tell" for certain foods: The high prevalence of poliomyelitis in both Coney Island and Rockaway Beach, two resort havens full of junk food and whatever served as the Whack-a-Mole of its day. “In proportion to its resident population, Coney Island, which forms the southern end of Brooklyn, has suffered quite heavily,” according to the health department report. “Here there have been two more or less clearly defined foci with a few more scattered cases. The greater part of these has been in old houses under bad sanitary conditions, and neither rodents, flies or insects would be excluded.” You can almost sense the foreclosing of fresh thinking here as the focus returns to the old favorites -- rodents, flies or insects.
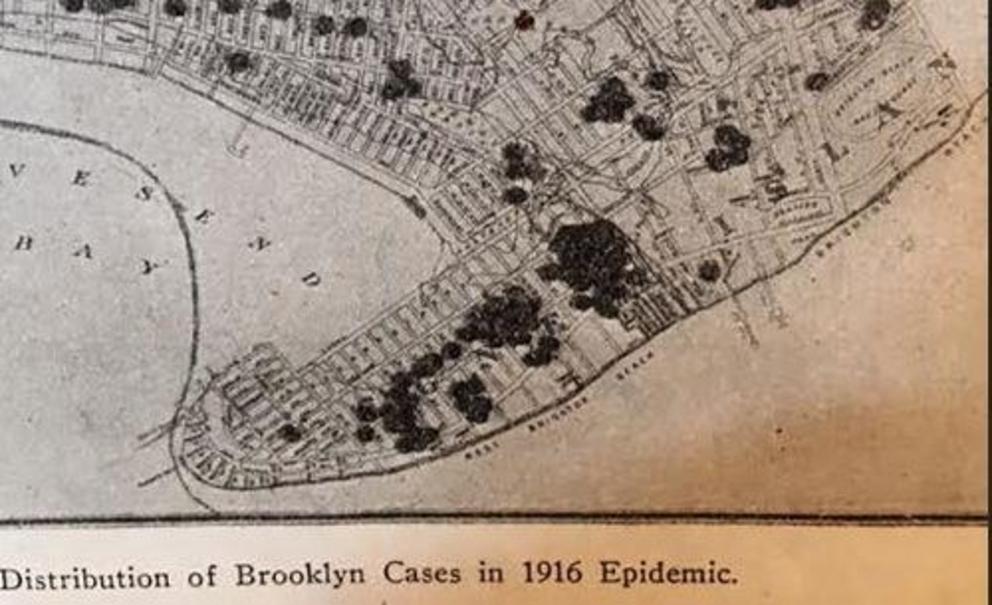
“One other locality in the Borough of Queens which suffered rather heavily was the extensive summer colony which extends along Rockaway Beach. Many cases appeared here in three or four poorly defined groups. Here the conditions are similar to Coney Island except that the houses are of better construction and in somewhat better conditions. They are, however, old and not of the small type with open-air space below mentioned in connection with Staten Island.” So rodents, flies and insects don't seem to be as likely here, yet the thing they do share, and that others have mentioned repeatedly -- certain kinds of food -- literally has dropped off the map.
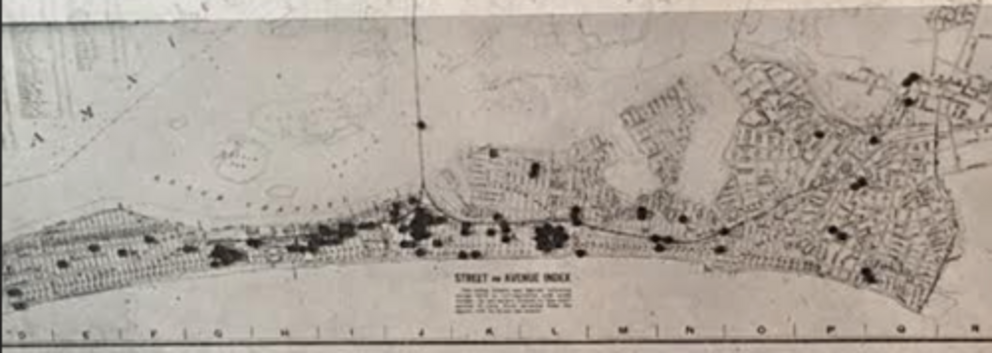
Several folders I examined mentioned families going to Coney Island over the Fourth of July 1916 holiday (the peak day for the epidemic was July 30); one said their child got sick “possibly the day they visited Coney Island.” Brooklyn's extensive streetcar system made it easy to get to the beaches; trains brought kids from as far as Pennsylvania for a Disney-style day trip. Suddenly that summer, they stopped.
Summer 1916 was when a new company opened its first stand on Coney Island.
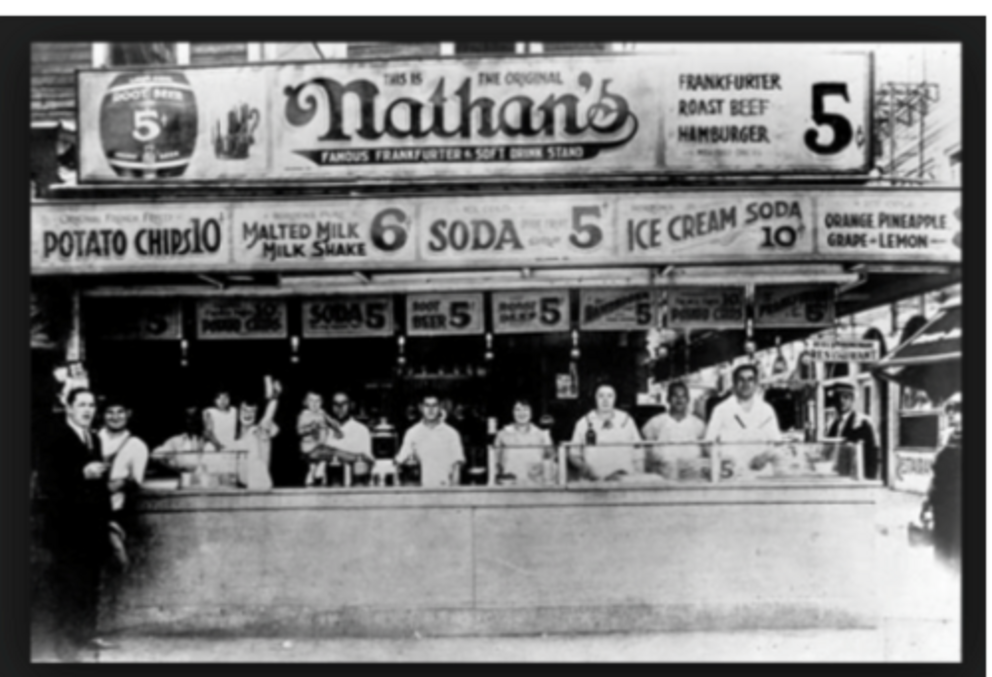
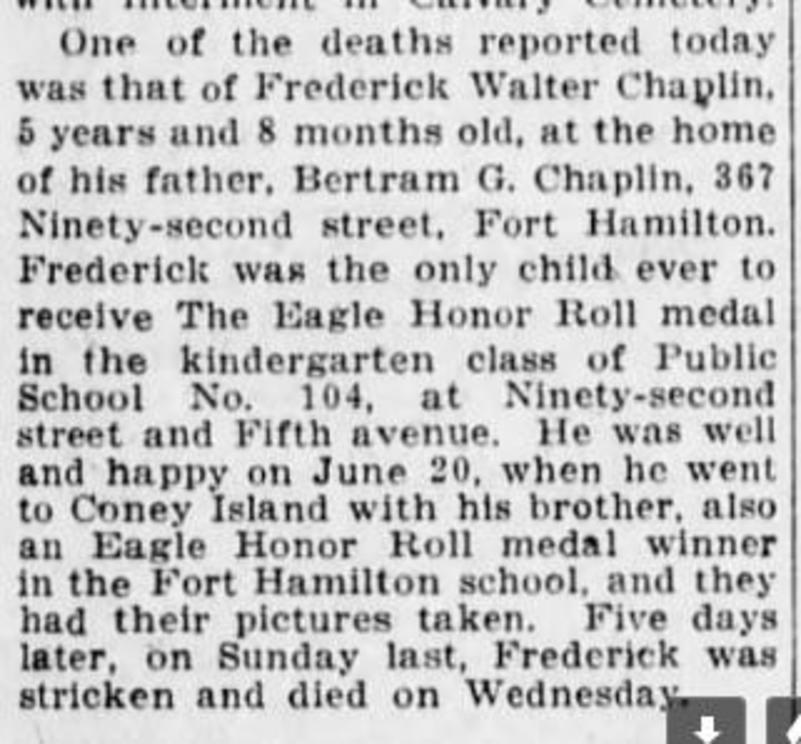
One can’t help thinking of ice cream, soft drinks, candy, fruit, and baked goods like hamburger and hot dogs buns -- all represented on the Nathan's sign (and notice the child at left-middle). Here is an obituary from the Brooklyn Daily Eagle; I’ve read this many times. The treasured kindergarten Eagle Honor Roll medal he was the only one “ever to receive” – an award likely to have been forgotten in the onrush of a full life -- seems an especially poignant memento of a foreshortened one:
--
Please, skeptics, don’t’ say I said that Nathan’s Hot Dogs opened in 1916 and promptly caused the worst polio epidemic on record, or that Coney Island and Rockaway Beach, which received well beyond the normal swell of visitors that hot and scary summer, were ground zero. These could just be places where children with active polio infections congregated and ate and shared food and drink and infected each other with the virus. End of story. (Measles at Disneyland, the prelude.) But then, why isn’t there more evidence of school-based infections in May and June? The presence of polio by early May 1916, sans vaccination, should have spelled more trouble and left more markers of contagion on the city’s schools.
Yet Emerson wrote: “On June 24th, in order to give immediate reply to many anxious inquiries and suggestions as to the part played by schools in the spread of the disease, a press bulletin was issued, pointing out the facts that 90 per cent of the cases were in children under school age, that the cases were not limited to any one school district or to children of the same classroom.
“The school term ended on June 30th. At the same time there was issued a special bulletin for parents, emphasizing the known facts which would be of service in preventing the spread of the disease in homes. The presence of the virus in the discharges from nose and throat, and bowels of infected individuals, the probability that atypical and non-paralytic cases were as dangerous and as numerous as the paralytic cases, and that little value or protection could be expected from the use of so-called antiseptic gargles and nose-sprays, were explained.” So Frederick Chapin still had 10 more days of school when he went to Coney Island on June 20, but it was that visit that stood out to his family.
Some children may already have been immune, and many developed inapparent or mild cases, but that doesn't quite explain the strange pattern of poliomyelitis. Was there some X factor or co-factor hidden in these patterns, in the black dots strewn along beach towns, in Mrs. Franklin’s ice cream shop, in the letters flooding the health department, in the realization that “provision shops” looked like loci to unbiased observers? Humor me and reread this passage by Dr. Emerson. Its significance got past me many times.
“There seems to be a well-marked tendency for cases in Manhattan to appear in the immediate vicinity of stables, groceries, meat or poultry markets, lunch rooms, delicatessen shops and bakeries or macaroni factories. … It is surprising with what regularity one or the other is found in the building next door to a house in which poliomyelitis has occurred. Others who have also examined the same districts with an unbiased mind, seem always to believe that cases range themselves with a definite relation to shops of this type. It has been repeatedly pointed out in earlier epidemics that stables are often associated with cases of poliomyelitis. This has been undoubtedly true in New York during the present summer, but the other association with provision shops has also forced itself upon our attention.” (italics added.)
Of the millions of words put together about polio, these may be among the most important and at the same time the most overlooked, because they point to a signal picked up by the health department for the first time in 1916 -- a straight-on correlation with food, and certain foods in particular, the kind Dr. Emerson laughed off just a few pages earlier. Let's repeat for emphasis. This observation was "surprising." It was "definite." It occurred "with regularity ... repeatedly ... always." It "forced itself" upon the attention of on investigators who were looking the other way, back toward their comfortable hypotheses of stables and rats and filth and flies. Even the fact that the Bronx cases were in "one of the somewhat better districts" argues against that comfortable view.
And while the association had been made before, the "well-marked" evidence was new. Rhymes with clue. It's almost as if Emerson had gotten so used to considering it nonsense that when it came up in a much more credible context, he stuck with his bias rather than looking at the information afresh.
And where have we seen this evidence before? Emerson is describing the world of 1295 Gates Avenue and Mrs. Frankin and Lettie Caruso and Peter Pinchero and early May 1916, isn't he? Yes, but it’s more than that. Just as the Coney Island and Rockaway tolls took no account of visitors who lived outside the beach neighborhoods, like Frederick Chapin, the association with these food emporia was probably stronger than it appeared by counting only the buildings next door and down the block. This surprising, convincing, repeated, new evidence was discounted, derided, forgotten. Yet there was a signal here, a signal that sank beneath the waves of mainstream epidemiology, drowned in large part by the laughter of “experts” like Haven Emerson and, perhaps most surprising, their lack of intellectual consistency and rigor. Let’s see where it takes us.
4.
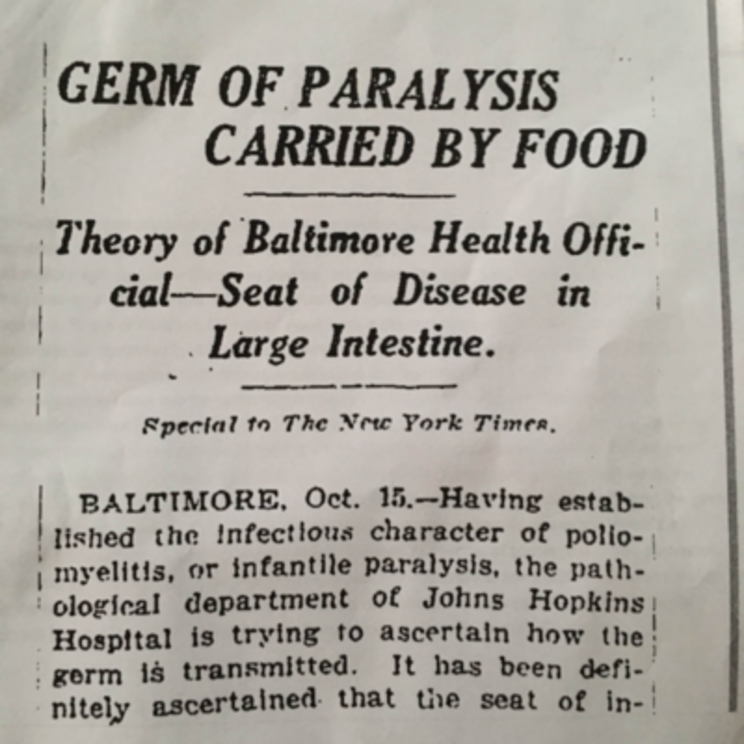
Public health officials had enough to do trying to cope with the polio epidemic in the summer of 1916 without having to listen to nonsense put forth by provincial people in Baltimore, of all places. “Germ of Paralysis Carried by Food – Theory of Baltimore Health Official – Seat of Disease is Large Intestine,” The New York Times reported October 15, after the epidemic had subsided but while sensitivities to the failure to contain or comprehend it were evidently still raw. The New York experts must have been so not thrilled to see this theory resurface.
The short article cited a Dr. H.T. Burrows of Johns Hopkins and Dr. J.F. Hempel of the Baltimore Health Department. “Dr. Hempel has a theory that candy, ice cream, fruit, and other uncooked foods that children eat, are primarily responsible for bringing the germ into the system. That theory will be fully tested when the physicians have completed their transmissions experiments.”
Nope. That was not gonna happen. The very next day, Dr. William H. Welch, head of the Hopkins medical faculty, fell on his sword under what must have been intense pressure from the New York City health establishment: “Denies Hopkins Rumors: Stories of Startling Discoveries in Paralysis Untrue, Dr. Welch Says." The Times quoted Welch saying that “the work which the Hopkins pathologists were doing in association with the physicians of the city health department on infantile paralysis had not developed anything that would change any views of the disease previously held.” Furthermore:
Welch was having none of it, especially as regarded children's favorite food: candy. Writes Samira Kawash, who calls himself the Candy Professor: “The official reply to Burrow’s and Hempel’s claims was swift and brutal. The very next day Johns Hopkins Professor of Pathology Dr. William Henry Welch, perhaps the most powerful medical authority of the day, contacted The Times to defend the reigning medical orthodoxy. Welch’s refutation of Burrows and Hempel singled out the particular claim connecting infantile paralysis and candy: 'The statement that the disease may be transmitted through candy is entirely gratuitous.' Welch could have more diplomatically called Hempel’s theory 'unfounded,' or 'incorrect' or even 'wrong.' Instead, Welch seemed to make a point of expressing scorn for the poor medical man who dared challenge the orthodox establishment. It was, according to Dr. Welch, preposterous even to wonder whether candy had some relation to polio.”
--
How many times now have we read about candy, ice cream, baked goods, fruit and so on being suspected in poliovirus contagion? I count four -- the letters to the New York Health Department that mentioned ice cream, candy, summer fruits and soda water, followed by cereals and canned foods; the observation recorded by the health department itself that stores selling "provisions" like ice cream, candy, and baked goods seemed to be new epicenters around which contagion clustered (along with stables, meat shops and so on); Sandler's no-polio diet in 1948 that forbad "sugar and foods containing sugar, such as soft drinks, fruit juices (except tomato juice), ice cream, cakes, pastries, pies, candies, canned and preserved fruits"; and now some crackpots at Johns Hopkins and the Baltimore Health Department who were about to put their ideas about "candy, ice cream, fruit and other uncooked foods" to the test when they got swatted down. Each seems to have a slightly different rationale for being linked to polio -- blood sugar fluctuations, observations about how cases clustered, concerns about raw and uncooked food, simple and easily dismissed associations made by ordinary citizens like the grandpa who bought his daughter ice cream before she got sick. So the reasons varied, yet they converged on the same vectors.
But by October, as the Times’ 24-hour turnabout shows, food and poliomyelitis was a politically incorrect correlation -- perhaps today's phrase for "gratuitous." Ice cream causes polio? It was dangerous to your academic standing, to your risk of being taken seriously by the powers that be, to even speak about such things. It still is. But there is much more to be said for it.
5.
. At 6:45 p.m. on Saturday, July 1, 1916, a 25-year-old Philadelphia man named Charles Epting Vansant lay on the manager’s desk at the Engleside Hotel in Beach Haven, New Jersey, and bled to death. A few minutes earlier, taking a dip before dinner, he was happily playing in shallow water with a Chesapeake Bay Retriever. When the shark struck, bathers watching the scene at first thought he was still splashing with the dog. That briefly delayed coming to his aid, but it probably didn’t matter. The shark tore the flesh off his thigh in one bite.
Already, fishermen had reported an especially active “shark summer,” with hundreds swimming in the mid-Atlantic. But the idea that one would attack humans on a populated beach so near to shore.? Not bloody likely. Even after it happened, the powers that be, concerned about summer tourism, played down the threat. The sharks weren't listening: Several more attacks occurred, immortalized in Steven Spielberg’s Jaws.
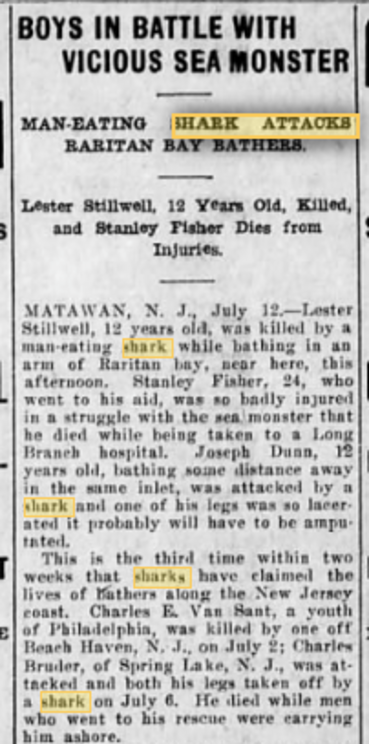
Sharks were not the only plague at the water's edge that summer before America entered world war. It's where the polio epidemic surfaced -- in the hardscrabble world of Pigtown, not far from the East River, where first one child and then another was pulled under by the circling virus. The annual infant mortality rate in New York City was already 12.5 percent, meaning every year one child in eight died before their first birthday. Polio was a peril, but so was diphtheria, whooping cough, cholera, and the “summer complaint” of childhood diarrhea that no doubt stemmed from the bad effects of sweltering heat of food, especially milk. (And this was an especially hot summer, the kind that drew bathers to the shore and sharks to bathers). A few years before, free "milk stations" had been inaugurated to make sure pregnant women and children got clean fresh milk.
The monster-from-the-deep analogy, in which a cunning killer attacked children, is not stretching things. After 1916, children were told "to regard [polio] as a fierce monster that lurked in the damp hollows of their experience," wrote Jane B. Smith. In a 1934 article titled Death Walks In Summer, B. Davies called the disease as "a grim terror... more menacing, more sinister than death itself."(1)
When health department workers went door to door later that summer, they counted up 29 polio cases from the month of May -- the plurality clustered around the Gowanus Canal, as we've noted. Plotting them on the map, they identified an epicenter for the entire epidemic – “a thickly populated Italian section, bounded by Fourth Avenue, Nevins, Carroll and Union streets.”
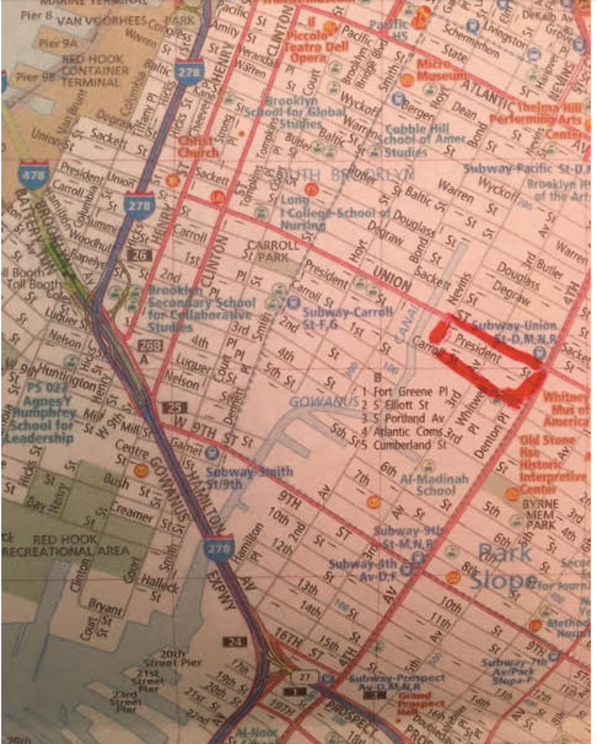
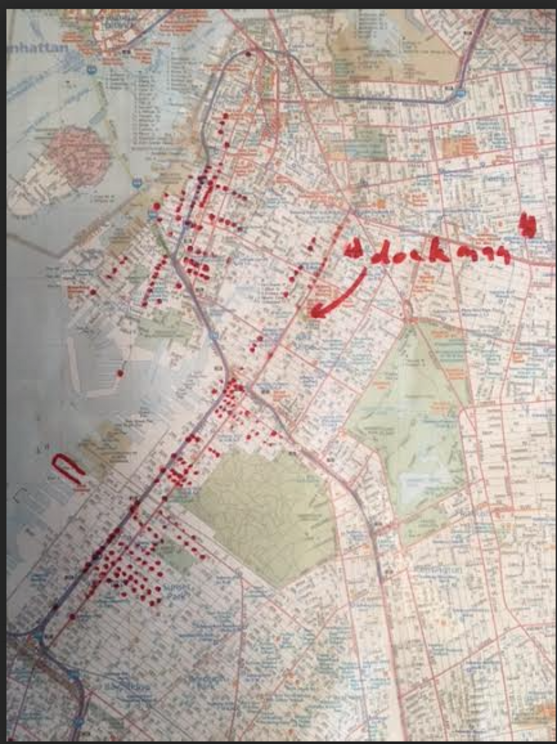
Because these and other early cases were close to the waterfront, where rats ranged freely among the cargoes and warehouses full of foodstuffs, the department decided to separate them out and take a closer look. Of the 1,403 cases of death and/or paralysis recorded in Brooklyn by July 15, they plotted 119 they considered close to the waterfront. The health department noted the remarkable fact that of those 119 cases, “91 occurred on six streets, namely 3rd and 4th and 5th avenues, 17th and 20th and 21st streets.” The total ranged from 9 to 34 cases on each street, with the most on Fourth Street. I took that list, added back any street with at least four cases to try to catch patterns but not isolated cases, and, armed with the amateur historical epidemiologist’s best friend, a red felt-tip pen, made a dot for each.
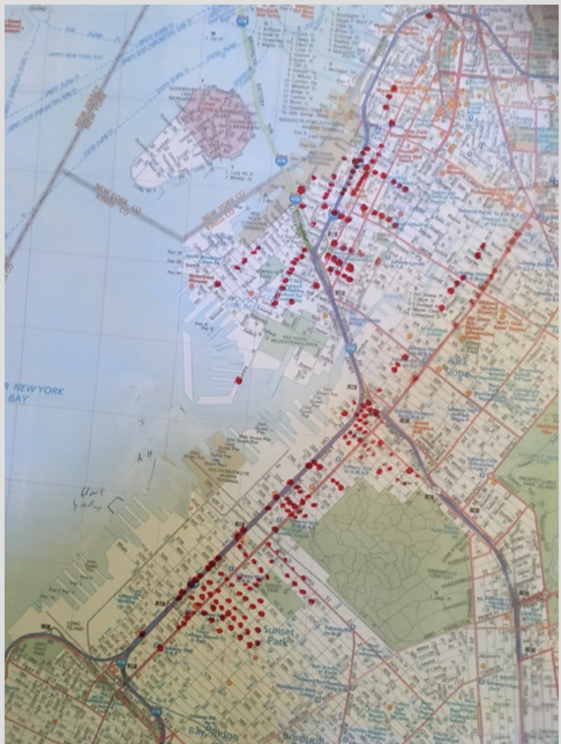
Well now. These dots connected, at least in my mind, in a new and interesting way. The Gowanus Canal, I realized for the first time in a couple of years of staring at it, is a classic McGuffin – it seems important at first but it's irrelevant to the plot (like Janet Leigh running off with her firm’s money in Psycho and straight into Anthony Perkins at the Bates Motel. The theft had nothing to do with it). Gowanus was just an Italian neighborhood proximate to the docks.
Example: A girl who lived at 345 Third Street, in the Gowanus Canal cluster, came down with scarlet fever in April 1916. The father’s occupation was listed as “dockman.” To go to work, he probably walked to the corner of Fourth and Union, got on the Fourth Avenue subway and hopped off at the Bush Terminal dock at the lower left, where so many other dots form a grid. In the photo below, "dockman’s" home is marked by a circle. It’s just three blocks away from the epicenter of the epidemic.

And here it is on the bigger map:
It’s also possible that "dockman" worked at the Red Hook docks to the left (west) of his home, or further north in Greenpoint, although the mass transit lines point to Bush Terminal. (On the Waterfront starred Marlon Brando as an Italian dockworker in Red Hook – you can see the Red Hook container terminal at the upper left of the photo above -- although the movie was actually filmed in Hoboken.)
And why does any of this matter? They point like an arrow to this fact: As of July 15, something about families who lived near and/or worked on the docks in Brooklyn had created a risk for polio in their children. But what was the risk? Simply the spread of the virus along the most prominent routes of travel? That's possible, but why did polio cluster around those particular docks and the arteries leading to and from them, rather than more randomly along the water? And how does it fit, if it does at all, with our observation about certain kinds of food as a clue to the nature of the epidemic outbreak
To answer that question, we need to back away from our closeup and adopt a much wider view, both in time and space. As a slightly lesser light than Einstein, Sherlock Holmes, put it, “In solving a problem of this sort, the grand thing is to be able to reason backward. That is a very useful accomplishment, and a very easy one, but people do not practice it much. In the everyday affairs of life it is more useful to reason forward, and so the other comes to be neglected.”
Fasten you're seatbelts, we're heading on a 4,884 mile excursion.
6.
“The summer wind came blowin’ in from across the sea …" (Summer Wind by Henry Mayer and Johnny Mercer, 1965)
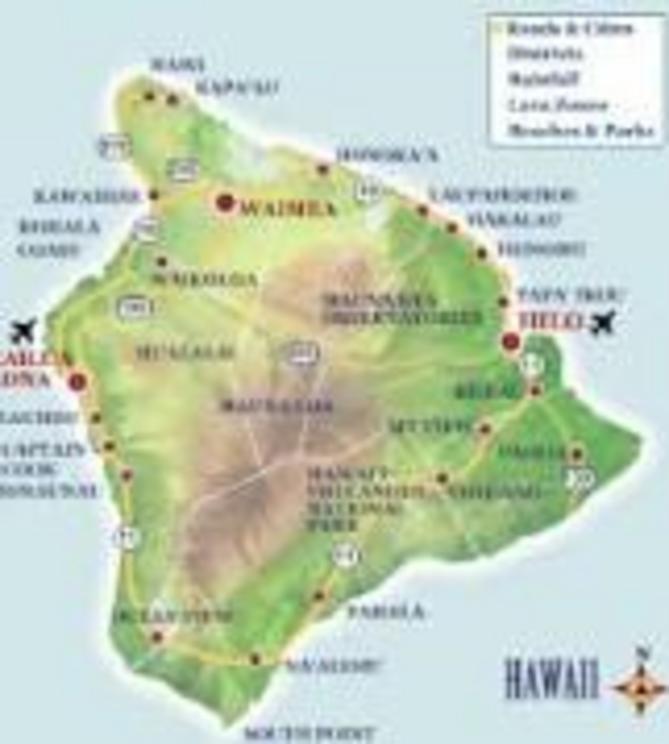
The Big Island of Hawaii rises out of the Pacific like a ridge-backed dinosaur, its volcanic spine splitting the island between the arid leeward side and the green, rain-drenched windward half. The westerly breeze, unimpeded across vast expanses of ocean, brushes up against the spine and pauses, pulling up moisture from the ocean and the saturated soil and pouring it back down. An average year brings up to 200 of rain to the eastern side, making it one of the wettest places on Earth – three times the annual rainfall of, say, Brooklyn.
--
Sugarcane has been called the thirsty plant, in need of endless water to feed its roots and stalks and leaves, as the grass – its technical classification – climbs ever higher in tightly bunched rows, reaching twice the height of humans. Even the light gets crowded out. A warm and wet climate, like much of Hawaii, is a perfect place for sugarcane to thrive.
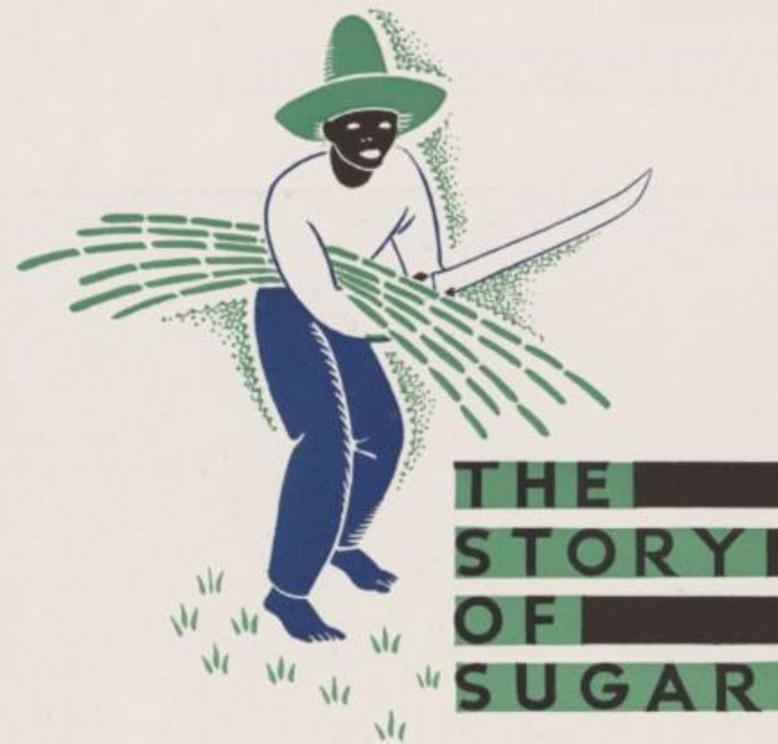
Unfortunately, it’s not a convenient place – nor is Cuba or Brazil or the West Indies or Puerto Rico. Cane is grown in places that can’t afford it, then shipped to places that can, a Third-to-First-World transaction that fed a sordid history. Slavery arose in significant measure out of the need for someone to do the backbreaking work of chopping down and hauling the stalks to the nearby mill, where more hard labor fed it to the grinders, crushers, boilers and separators. Accidents and death by exhaustion were not uncommon, but the labor was expendable.
The end result of all this planting, tending, harvesting and milling was not even the end result -- just a thick brown mixture known as raw sugar. This is not the kind you tear open and dump in your coffee at Starbucks; it is unsafe to eat, full of dirt and organic matter mixed with fertilizer and pesticides in a coating of molasses; even the stray button or coin was occasionally dropped into the mix.
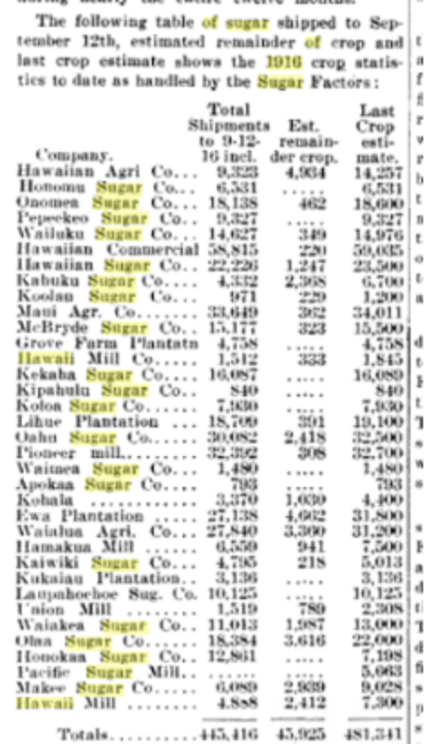
The raw sugar was loaded onto freighters bound for the continental U.S.. A portion went straight to a sugar refining plant in Crockett, California, but most – by rail, or through the Panama Canal, or across an isthmus in Mexico, or around Cape Horn – made its way to the great East Coast refineries in New York, Philadelphia and Boston. A group called the Sugar Factors did business for the plantation owners, selling contracts for the year’s crops to distributors in San Francisco and the East Coast cities. At the docks the cargo was unloaded and conveyed to the nearby refineries-- the sugar freighters of the American-Hawaiian Steamship Company for many years had their own pier, the world's largest, at the Bush Terminal in Brooklyn.
The refineries -- half a dozen ringed New York Harbor -- put the raw sugar through the wringer all over again – a brochure from the 1933 World’s Fair lists 71 steps from arrival to packaged product. A good deal of the “refining” is simply designed to turn the sugar white, an ironic accomplishment given the black lives laid waste along the way. (I had to quit reading the book Sugar because the description of how slaves were treated on the sugar plantations was so horrifying). After the Domino Sugar Factory stopped operating a few years ago in Brooklyn (its huge Domino sign was an icon on the waterfront), an art installation in its cavernous ruins called the Sugar Sphinx, by Kara Walker, spoke to that history. The New Yorker called it “triumphant, rising from a kind of half-world—the shadowy half-world of slavery and degradation.” (Full title: “A Subtlety, or the Marvelous Sugar Baby – An Homage to the Unpaid and Overworked Artisans Who Have Refined Our Sweet Tastes, From the Cane Fields to the Kitchens of the New World on the Occasion of the Demolition of the Domino Sugar Refinery Plant.” That pretty much tells the story, except for the fact that sugar as a food is now recognized as worse than worthless. The world would have been far better off if it left the cane alone.)

Even after slavery, the paternalistic and colonial impulse remained. That 1933 Jack Frost brochure shows jaunty dark people gathering up the cane, referring to them as “natives” who “cut down row after row of the cane with a machete” and load it onto horse-drawn wagons (in 1933!). It sounded almost pleasant, “the picturesque acres of green-leafed ‘bamboo’ reeds stretching as far as the eye can see.”
Things were somewhat better in Hawaii. The plantations relied not on slave labor but on coaxing laborers to immigrate. most often from Japan or the Philippines. The first Hawaiian plantations grew up in the mid-1800s. Their American owners – many of them former missionaries – became power players with mercenary interests of their own, leading directly to the overthrow of the indigenous monarchy and the slow incorporation of Hawaii into the United States. By 1900 trade relations were so advantageous that it made sense to cultivate more marginal acreage.
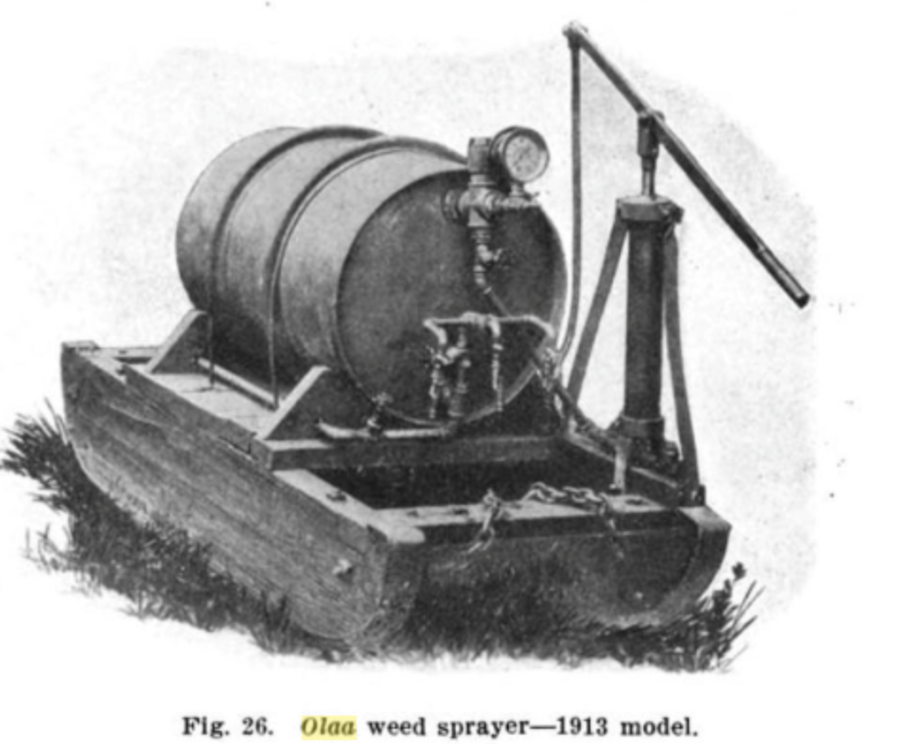
Chief among them was the Olaa plantation, which, while on the rainy side of the dinosaur’s backbone, was iffy real estate. The volcanic soil was porous and uneven, the ground on the lower mountainside where the cane was planted sloped inconveniently, and the immense rainfall meant that everything, not just the cane, grew like Topsy. Weeds ran wild, more than could profitably be pulled by sheer human effort over the long, two-year growing season.
By 1913, barely a decade into the Olaa enterprise, the bottom line looked bleak. The owners got rid of the current manager and went all-in on an unlikely savior – C.F. Eckart, head of the experiment station of the Hawaii Sugar Planters Association. His new salary was rumored to be an astronomical $12,000 a year -- $290,000 in today’s dollars. His mission was to cut costs by making the crop less labor-intensive and, while he was at it, increase the yield.
Desperate times called for desperate measures. Eckart set to work doing what he had been paid so handsomely for. He experimented.
7.
Along with his generous salary, Charles F. Eckart reaped other benefits that went with being a Hawaiian plantation manager in 1913. In vivid contrast to his former life as an experiment station official, he lived in a mansion two miles from the Olaa plantation office. A book about a subsequent Hawaiian sugar strike by Masayo Umezawa Duus captures the world that awaited him as he approached for the first time his new home with its immense veranda, stables for riding horses, and distant view of the Pacific.
"The mansion still stands,” Duus wrote in 1987, “its landmark a huge banyan tree that is said to date from the era when native chieftans held power. Along the private road leading to the mansion dozens of tall coconut trees pierced the sky. The three-story white structure sits on the crest of a rise surrounded by an expansive lawn.” Although it’s decrepit now, the place is imposing enough to “hint at the status and power of the plantation manager, who the Japanese laborers likened to a daimyo, a feudal lord, and whom they likened to the ‘owner’ of the plantation.”
Eckart barely had time to settle in. He quickly set about addressing Olaa’s crop woes with expertise and tools developed at the experiment station. The root of the problem at Olaa was the rainfall on the windward volcanic slope of the Big Island, which could reach 200 inches a year and allowed weeds to overtake the crop itself. The manpower required to keep ahead of them over the two-year growing season threatened whatever profit the plantation might eke out. At the experiment station, Eckart and a fellow researcher, H.P. Agee, had been working on a solution -- literally.
An arsenic solution.
“New method of weed control,” the journal Sugar reported in June 1915, after that solution had been widely implemented on Olaa’s sugarcane fields. “The system which would appear to be the most satisfactory is that of Agee and Eckart, in which the weeds are sprayed with arsenite of soda. Two special spraying apparatus have been invented, the spread sprayer and the knapsack sprayer.”
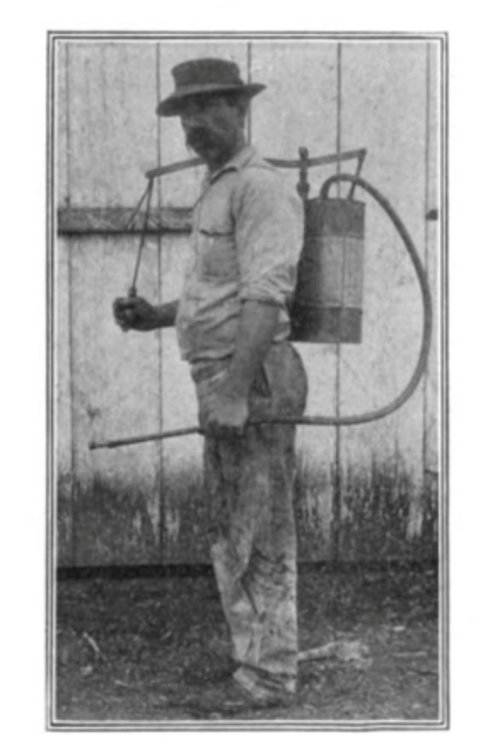
Early concerns about the method had been alleviated, the article said. One was whether the arsenic would kill the golden goose – the sugarcane – and not just the weeds. It didn’t: “Experiments carried out in Olaa, in which arsenic was applied to the soil between the rows at the rate of 5 lbs. per acre each week for six months, showed that the arsenic had no injurious effect on the growth of the cane plant.”
If you think the second issue might be whether the arsenic posed any problem for those who would ultimately ingest the sugar in New York, Philadelphia, and Boston – you would be mistaken. “The second problem, as to whether the poison employed in the process damages the cane itself, has also been answered in the negative. It is true that, even with the best apparatus, small quantities of the spray cannot be prevented from coming into contact with the leaves of the young cane occasionally. But this is not a matter of importance, because it is at most occasions a slight check to the cane, from which it recovers entirely within a few weeks.”
What a relief – to the owners, at any rate. You could spray thousands of gallons of an arsenic solution on fields for two years and still harvest a healthy crop. Sure, a lot of arsenic got into the sloping, rain-soaked soil, and who could help sloshing a little onto the sugarcane plant from time to time? Meanwhile, the dead weeds were left where they lay to decompose. The point was, the plant recovered. It was not a matter of importance.
Here we are, then, in June 1915, with arsenic being sprayed for the first time – ever, anywhere, as far as I can tell – on a sugarcane crop. “It may be said that this method of weed control already has passed the experimental stage,” the article stated, “as it has been adopted as a part of the normal field work in the extensive plantation at Olaa.”
The article gives the formula – 5 pounds of arsenite [an arsenic-based compound] to 100 gallons of water. Eckart, the article said, was ordering as much sled-spraying as possible, with a “light hand-spraying to touch up the spots that may have been missed by the sleds.” According to an unnamed authority, “by observing the proper rules and ordinary intelligence, spraying can save a plantation in labor from $15 to $30 per year per acre.”
This process appears to have gotten under way not long after Eckart’s arrival in 1913. Given the two-year growing season, followed by harvesting, hauling, and milling at a nearby factory, the first crop that got the full arsenic treatment was doubtless the one that arrived at East Coast early in 1916.
I’m always interested in the first time something is tried, because, almost by definition, no one knows what the hell he or she is doing. That’s why they call it an experiment. It’s one thing to try arsenic out at the experiment station, another to spray thousands of gallons on thousands of acres will yield thousands of tons of sugar to be consumed thousands of miles away, with no sense of caution – and certainly no notice to the East Coast refineries -- that things might be a little different this year.
Too much arsenic? If so, where? In the soil? In the leaves? In the stalk? In the sugar? How about variables like rain, volcanic soil, gradient, uptake characteristics of the cane and the arsenic compound? And how about the machinery developed just for the job, which while triumphs of invention for their day might not pass muster in 2016. What about the consequences of mingling “poison,” food, and the potential for human error, with little to no oversight from anyone but those who stood to profit?
Seriously, what about it? Next week we’ll examine those questions in depth.
8.
Spraying arsenic around food doesn’t seem like a very good idea to me, but if you read the scientific literature of the time, you start to think it's like sprinkling a little parmesan on your spaghetti. I was about ready to try a spoonful myself (you could do that too for many years – it was called Fowler’s Solution!). So I reached out on AOA to find someone familiar with toxicology to give me a more modern understanding. A reader with an advanced degree in environmental toxicology got in touch and proved to be terrific. I gave her all the information I had about the use of arsenic on the plantation and she gave me her feedback over several exchanges.
She displayed the straightforward and careful approach that I associate with good science, and I’m going to share what she said pretty much verbatim – saving some for later when it’s more appropriate. My interest was whether enough arsenic could have made it from Olaa’s cane fields through the harvesting and milling and refining processes to become a potential factor in the 1916 epidemic. I sensed she would tell me if this seemed like a crazy idea, so I waited with more than usual interest for her e-mail to pop up in my inbox. It read:
--
Hi Dan – I would not discount the presence of arsenic (used as a pesticide) in the sugar. Here are some thoughts on what you sent me:
-- Just as background, arsenic is sometimes a metal and at other times a metalloid. This property makes it very versatile in the forms it can take – arsenic can form a number of different compounds.
-- Arsenic is an immune suppressant as are heavy metals in general. Arsenic binds to sulfur compounds and impairs enzymes; it also competes with phosphate, which is needed to synthesize ATP to produce energy.
-- Arsenic does act quickly, and a child would get a disproportionately large dose from a “regular” serving of whatever sugary food was eaten, so arsenic could act relatively quickly to suppress a child's immune system.
-- Regarding the formulation of the arsenic spray in Hawaii: What they were doing with the caustic soda (NaOH) and heat is making white arsenic more water-soluble, so that it would remain in solution – i.e. spray easily and not settle out. That would increase its utility as a pesticide by improving its “flow” and its “shelf life.”
I don’t have any idea what spraying equipment looked like in 1916 but even today it’s difficult to hit only the weeds and not the crop with pesticide spray. (I shudder to think of the occupational exposure.) Moreover since the arsenic pesticide was highly water soluble it would have been carried into the soil and been available for uptake by the roots of any plant that was nearby. So yes the sugar cane could have been contaminated by inorganic arsenic. I need to do a little reading on arsenic uptake in plants to understand this better. It’s kind of the opposite of using plants to clean a Super Fund site: in that case the plants are destroyed after binding heavy metals in the soil, while here the plants were refined into food.
--
How helpful was that! I replied:
Thanks so much.
-- Here's a link to a discussion of the spraying technology at olaa.
-- Here is a discussion of the effect of arsenic on the soil in Hawaii
-- I've found various and quite different discussions of whether sugarcane takes up arsenic. There was a study around 1933 in Hawaii that said a field on which arsenic was used had no more arsenic in the plant than a field that was arsenic-free. But I've also read about how rice -- which has a major arsenic-uptake problem -- and sugarcane are two of the major plants that take up silicon in large amounts. In the case of rice, the silicon transporters mistake arsenic for silicon and take it up. I have no idea if that could happen to sugarcane.
-- Here is an article that suggests quite a bit of arsenic was taken up in sugarcane in Brazil”
--
Her response:
Hi Dan – I have done a little more reading on arsenic and here are further thoughts (four journal articles attached).
- The form in which arsenic was sprayed onto weeds is highly bioavailable to plants, which is why it kills weeds so fast (in 1-2 days). It’s also highly bioavailable to humans. I would have to believe that at least a small amount of arsenite sprayed onto weeds would have made contact with the proximate sugar cane. In addition, the “splashing” effect of rain would have carried some arsenite from surface soil onto surrounding plants including the nearby sugar cane. That arsenite could have been taken up by the cane.
- The paper from the USDA assumes that the arsenite was washed out of the soil, and that may very well be correct given the hilly terrain and porosity of the soil. But that takes a little bit of time, so the arsenite is available to the cane roots for some brief period of time (a week? a month? three months? I don’t know). Also the plants down the hill would be exposed to arsenic migrating from uphill so there’s a “gradient” effect.
- The killed weeds were left in place to decay, which would have caused the arsenic in their tissues to be recirculated back into the soil. That becomes a “secondary” source of arsenic exposure, which would have been available to the sugar cane roots. This variable was not included in the USDA paper on the fate of arsenic in Hawaii soil: it assumed the only source of arsenic was the original spray.
- The Brazilian researchers found that sugarcane does take up arsenic into its tissues and that more is found in the cane than in the leaves. So it is entirely reasonable to assume that arsenic was assimilated by the sugar cane and made it into the raw sugar.
Regarding the growing season: Hawaii is largely a year-round growing season, right? So the arsenic weed-killer would have been applied at regular intervals throughout the year. Cane is fast-growing so it would take up water and minerals in the soil at a rapid rate. The cane was taking up arsenic, but it also seemed to be growing normally (no mention of it being stunted or having small leaves, etc.) so the amount present wasn’t enough to interfere with growth. However the refining process would concentrate that type of small contaminant.
--
Well, this is quite educational, wouldn’t you agree?
I had read before that if a contaminant did get into sugarcane there could be hell to pay because the refining process would concentrate it. I must say that I still didn’t quite get that – I imagined a centrifuge spinning all the flotsam and jetsam to the side and leaving pure sugar crystals at the center, ready to fall neatly into one pound bags, pure as the driven snow. After all it had "refined"! So I asked:
“One more -- why would refining concentrate the impurity rather than remove it? I was assuming it was pulled out of the sugar itself ... ” Her answer:
--
The arsenic that was spread throughout multiple plants has now been concentrated into a small amount of sugar. Very roughly, it takes 80 tons of cane to extract one ton of sugar. So the arsenic in 80 tons of cane was released with the sugars. More of the impurities remained in the syrup than the crystals, but there would have been some in the crystals too.
--
To quote Leader of the Pack – yes, we see. I had a new appreciation for the uniqueness of sugar as a food – unlike a strawberry, which you “process” by planting, growing, and harvesting, sugarcane went through an amazing manufacturing process where it was refined. You could wash off a strawberry before you ate it, but you were pretty much stuck with whatever was in that bag of sugar.
This was insidious, for sure, if it’s true. Nobody would blame the sugar. They would ”blame” ice cream and candy and baked goods and soda water and cereal with sugar sprinkled on it. They would blame summer fruit (much of which was treated with lead arsenate pesticide, a topic to which we will return.) They would observe that cases clustered around provision shops that served and sold those foods began to look like important.
They did blame those things, they did observe those things. But nobody listened. Ice cream causes polio? Please!
It wasn’t the ice cream, per se, in this theory; the ice cream was just a vector. It was the arsenic in the sugar in the ice cream, and that was still only half the equation. The virus itself was the other half. Simple math would then explain why in a group of four children sitting on a park bench, one might develop poliomyelitis while the other three did not. One had the virus and one didn't; one had the arsenic exposure and one didn't; one had neither; one had both. The one who had both was the one at risk.
My toxiciological correspondent concluded: “This would have constituted a “light’ exposure (‘background’ is the wrong word because it implies the arsenic was found naturally in the soil, which it wasn’t, and ‘trace’ and ‘light’ aren’t good words either because they're not quantitative). But a ‘light’ exposure to arsenic could affect a human. Plus children are smaller than adults and thus more vulnerable to a given dose of toxicant than an adult, just because of body weight.”
So now we have a theory of the case. Next question: Exactly where did the sugar go, and what happened when it got there?
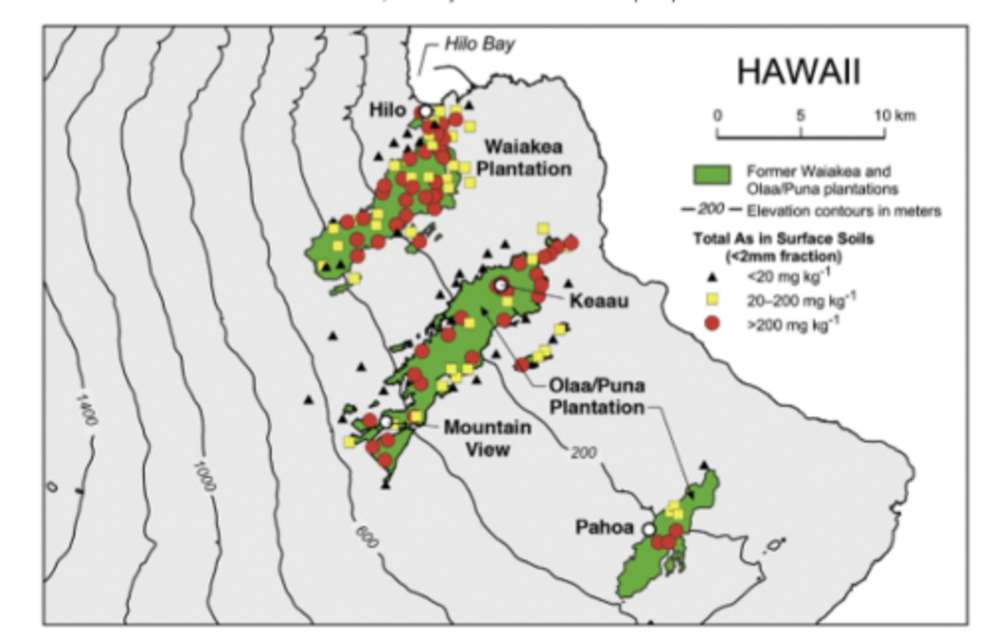
Oh, in case you’re wondering how much arsenic really got applied at Olaa, here’s a current map, decades after they stopped. They’re still trying to get rid of it. (Keeau is the modern name for Olaa.)
9.
Things were finally looking up for the Olaa Plantation. Eckart was reaping the rewards of his bold experiment to kill the plantation’s runaway weeds with arsenic rather than expensive human labor. The newspapers were full of plaudits.
“Olaa shows remarkable improvement,” the trade journal Louisana Planter and Sugar Manufacturer reported in September 1915. “The two years administration of the affairs of the Olaa Sugar Company on the island of Hawaii by Mr. C.F. Eckart, the former director of the Hawaiian Sugar Planters’ Experiment Station, have been marked by increases in yields and lowering of costs beyond the most sanguine hope of stockholders. The improvements have been general and while particularly noticeable in the data on crops, are, nevertheless, in evidence in the handling of labor and other activities of the company.” Although not mentioned, the arsenic treatment must have worked well.
On February 9, 1916, Eckart was quoted in the Hawaiian Gazette as saying that “the harvesting of this crop commenced on December 7, 1914, and completed on November 25, 1915. An unusually early start to the grinding season [at the mill] was considered advisable owing to the increased output of sugar expected. … Altogther 283,116 tons were harvested, yielding 32,308.22 tons of sugar.” So this 1915 crop, for early 1916 delivery, did so well that they had to start harvesting it early. Finally, the gods were cooperating. He told the press:
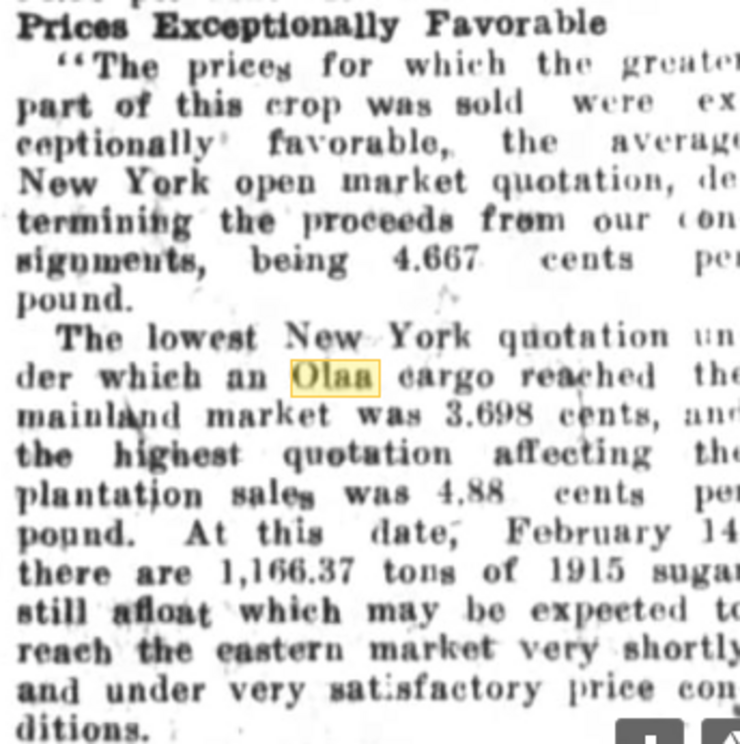
On February 25, the Honolulu Star-Bulletin was effusive: “Cost of Producing Ton of Olaa Cane Cut Almost 50 Percent.” Again, that had to be due in significant measure to the cost savings from the arsenic spraying, although it wasn't specifically mentioned. On May 19, the Hawaiian Gazette reported, “Olaa Sugar Company to Pay First Dividend. This Year’s Crop [for 1917 delivery] Probably Last One To Run Under 30,000 Tons; Yield Per Acre Grows.” Eckart outlined expansive plans to increase the size of the mill, add more railroad equipment, even buy 20 more mules – a total cost of $150,000. Once more, no mention of arsenic's role.
“War prices for sugar, good management, a constructive policy on the part of agents and directors, and a dogged determination to win have brought this great property through to this successful issue,” the paper said. Eckart was the toast of the planter’s world. But not for long.
In October 1916 -- just five months later -- the Louisiana Planter said that year’s Olaa crop [for 1917 delivery] was a disappointment. “Olaa Plantation, whose varying fortunes have been often the subject of comment by sugar statisticians and publicists, has further reduced its 1916 crop estimates [for 1917 delivery] … The new estimate is now 21,500 tons … The disappointment of the investors and of the stock market players is keen over Olaa’s showing this year.” You can see the figure below, fifth from the end.
In 2003 the Honolulu Star-Bulletin reported," State health officials have found high levels of arsenic in the soil at two community gardens in Keaau [Olaa] on the Big Island, and are offering free medical tests to residents to see if they have absorbed the potentially toxic element."
The article said "the probable source was herbicides sprayed on the local sugar plantation from 1915 to 1950." So the use of arsenic at Olaa apparently continued, though how the bagasse paper fit with that is unclear. And with American participation in World War I in April 1917, everything about sugar distribution changed. The American-Hawaiian Steamship freighters stopped their runs to the East Coast and were leased, profitably, to the Navy to carry troops and cargo. The few freighters that remained delivered the raw sugar from Hawaii to San Francisco for overland transport by train; eventually more Hawaiian sugar stayed on the West Coast instead of the inconvenient East.
If you accept the idea that arsenic in Olaa sugarcane led to a poliomyelitis outbreak, the one-year epidemic spike of 1916 begins to make more sense: a toxin (arsenic) found a vector (sugar) that delivered it to a place (Brooklyn) where a virus (polio) was circulating, triggering an outbreak of paralysis and death (poliomyelitis). The effect, in scientific terms, was amplification -- the toxin made the virus far more dangerous than either would have been alone. In lay terms, you could call it an Explosion.
The Star-Bulletin interviewed a 94-year-old who sprayed arsenic on those Hawaiian fields in the 1920s and '30s. "As a young man, Henry Texeira's fingernails and hair fell out, and his skin broke out in blisters when he sprayed an arsenic-based herbicide in sugar cane fields south of Hilo. ... The chemical he used was Penite, a brand name for sodium arsenite. 'People used to suffer like hell with Penite,' Texeira said. It's a form of sodium arsenite, an inorganic arsenic compound also known as arseneous acid, sodium salt and sodium meta-arsenite.
"Another brand name for the stuff," Texeira recalled, "was Kill-All."
--
*Sources and notes: Information about the sugar industry in 1916 comes from multiple sources including articles on newspapers.com and in specialized sugar journals. Case histories of Lettie Caruso, Mrs. Franklin and others are from the New York City Health Department archives of the 1916 epidemic at the American Philosophical Association library in Philadelphia. All names have been changed, which the library required as a condition for access. While I hesitate as a general rule to do that, it really made no difference in this instance. The chart showing the spike in the polio rate is by my colleague Mark Blaxill.
10.
As we prepare to follow the Hawaiian sugar harvest to the U.S. mainland in early 1916, a natural pause suggests itself. I’ve now presented the basic hypothesis: that arsenic applied for the first time ever to sugarcane fields anywhere, at the Olaa plantation on the Big Island of Hawaii, led to the first massive poliomyelitis epidemic in the United States.
It triggered the Explosion that ushered in the Age of Polio.
That kind of claim attracts critics who use words like "laughable." (Of course, laughable things can be true.) Over at Orac, Denice Walter commented: "Although I am often highly entertained by your speculation, I would be much more pleased with you if you took a few life science related courses at your local university." I responded: "Denice, I remain pleased that you are highly entertained. I fear that exposure to actual experts might reduce my ability to amuse you, so I’ll avoid it for now." (The claim here is that a non-scientist journalist such as myself has no business tackling a topic like this. I disagree.)
So perhaps it’s time to say a little more about how the theory evolved and where I am heading with it. In 2011, Mark Blaxill and I wrote a series called The Age of Polio: How an Old Virus and New Toxins Triggered a Man-Made Epidemic.
In it, we proposed that the invention of lead arsenate pesticide in 1892, interacting with poliovirus infections, kicked off the modern era of polio epidemics. Lead arsenate was created to fight the gypsy moth invasion around Boston that threatened to wreck the entire domestic apple crop. In a literal and metaphoric instance of the “butterfly effect” – seemingly minor and distant events leading to major disruptions -- a few moths escaped their enclosure in a back yard in suburban Medford, and before long turned into teeming masses undulating like black waves across suburban streets to devour fruit trees in one collective gulp. This story almost defies belief, but The Great Gypsy Moth War by Robert J. Spear brings it to creepy-crawly life.
Lead arsenate subdued the moth problem, but the association of the pesticide with poliomyelitis is hard for dispassionate observers (meaning those not wedded to virology as the explanation for everything) to dismiss. In 1893, the year after the first use of lead arsenate in Boston, two local doctors wrote a medical journal article, “Is Acute Poliomyelitis Unusually Prevalent This Season?” and very quickly established that it was unusually prevalent. “It would not have seemed worthwhile to report these observations had it not been that the number of cases observed at the Massachusetts General Hospital in September and October of this year [apple harvest time] is decidedly larger than usual. …” Putting together all the cases from four sources, they came up with six polio cases for the period August-November 1892, and 26 for the same period in 1893.
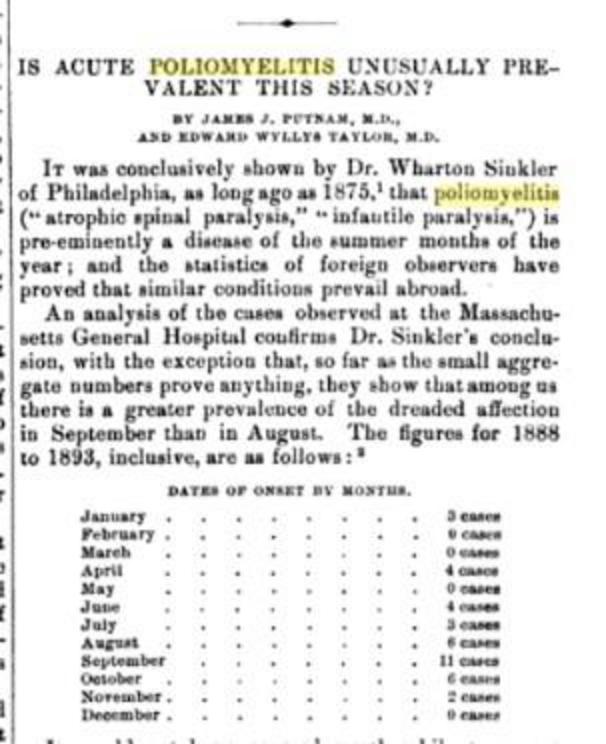
While that was an impressive rise, it could have simply been natural variation; sporadic cases were observed by medical professionals over the past several decades. Hence the question mark. But the very next year, 1894, in the Otter River Valley in Vermont, came the answer – an unmistakable poliomyelitis epidemic.
The account, a classic of medical literature worth reading in its own right, was provided by Dr. Charles Caverly, a Rutland physician who also happened to be the president of the state medical society – and was in the right place at the right time. The beginning is memorable and haunting, given what was to come and the fact that epidemic poliomyelitis was so unfamiliar in the United States that Caverly didn’t even call it “infantile paralysis” or poliomyelitis until later articles.
“During the month of June, 1894, there appeared in a portion of the valley of the Otter Creek, in the state of Vermont, an epidemic of nervous disease, in which the distinctive and most common symptom was paralysis. The great majority of sufferers were children under six years of age.” Hardest hit were the towns of Rutland and Proctor. There were 132 cases and 18 deaths.
This was not like Boston the year before. This was big.
As outbreaks became more frequent and much larger, “lead arsenate was proposed as a cause of polio epidemics early on,” as we wrote in 2011:
"In Massachusetts, where the compound was first used, the State Forester reported in 1912, under a section headed Infantile Paralysis: “In view of the fact that a feeling has been entertained by some people in the State that infantile paralysis has been caused in some instances by arsenate of lead used in spraying for the gypsy and brown-tail moths, the State Forester has caused a rigid investigation to be made in order to determine if there is any foundation upon which to base such fears.”
No there was not: “As a result of his research he is firmly convinced that the use of arsenate of lead has in no way been responsible for the existence of the disease [infantile paralysis], and apprehends no danger in the future from its use. Any anxiety concerning the danger from the use of arsenate of lead is entirely unwarranted.” Of course, today we'd say that anxiety was warranted simply because of the name of the compound!
On the other side of the globe, a New Zealand newspaper reported in 1914: “The oft-expressed opinion that the arsenate of lead spray on fruit is the cause of the prevalence of infantile paralysis will be discussed at the next meeting of the Upper Clutha Fruit-growers’ Association at Bannockburn. The association is taking steps to obtain the result of Government experiments regarding this matter.” (We have not found a follow-up report.)”
--
These concerns were never taken seriously. When you consider what was potentially at stake --half a million cases of death or disability a year worldwide by the 1940s -- that was worse than unfortunate. When DDT replaced lead arsenate after World War II, a handful of brave souls put forward the idea that pesticides, not the poliovirus, were the cause.
As Mark and I wrote in 2011:
--
In 1949 Drs. Morton S. Biskind and Irving Bieber published “DDT Poisoning – A New Symptom With Neuropsychiatric Manifestations” in the American Journal of Psychotherapy. “By far the most disturbing of all the manifestations are the subjective reactions and the extreme muscular weakness,” they reported.
In subsequent papers and testimony, Biskind linked DDT directly to cases of poliomyelitis – including a Dec. 12, 1950, statement to the Select Committee to Investigate the Use of Chemicals in Food Products, United States House of Representatives. He quoted another doctor that “wherever DDT had been used intensively against polio, not only was there an epidemic of the syndrome I have described but the incidence of polio continued to rise and in fact appeared where it had not been before.
“This is not surprising since it is known that not only can DDT poisoning produce a condition that may easily be mistaken for polio in an epidemic but also being a nerve poison itself, may damage cells in the spinal cord and thus increase the susceptibility to the virus.”
“Facts are stubborn,” Biskind concluded, “and refusal to accept them does not avoid their inexorable effects -- the tragic consequences are now upon us.”
The theory was also advanced by Ralph R. Scobey, who in 1952 gave a statement to the same House committee. Titled “The Poison Cause of Poliomyelitis and Obstructions To Its Investigation,” it described associations between harvest seasons, fresh fruit consumption, and polio epidemics.
The next year, Biskind made the link even more explicit: “In the United States the incidence of polio had been increasing prior to 1945 at a fairly constant rate, but its epidemiologic characteristics remained unchanged. Beginning in 1946 the rate of increase more than doubled.” Yet far from looking into a toxic etiology, he said, “virtually the entire apparatus of communication, lay and scientific alike, has been devoted to denying, concealing, suppressing, distorting and attempts to convert into its opposite, the overwhelming evidence. Libel, slander and economic boycott have not been overlooked in this campaign.”
--
More recently, medical writer Jim West has argued strongly for the link, and pointed to other risks from pesticides, like Parkinson’s Disease. In articles like, “Everything You Think You Know About Polio is Wrong,” he champions Biskind and the poison theory of polio.
“Today, few remember this poignant writer who struggled with the issues of pesticides, issues that Rachel Carson would be allowed to politely bring to public awareness nine years later, as the lead story in The New Yorker magazine and then as a national best seller, by limiting her focus to the environment and wildlife. Biskind had the audacity to write about human damage.”
--
Under our theory, that's true, but it's half the equation; the poliovirus is required as well to add up to poliomyelitis epidemics. And the implications reach far beyond polio: Toxins can amplify minor microbes into major epidemics to a far greater extent than is currently recognized.
With this paradigm in mind, let’s head back across the Pacific to Brooklyn. Early in 1916, sugar from Hawaii arrived at the American-Hawaiian Steamship Company dock in Brooklyn, which had recently been overhauled into a two-story behemoth.
You may recognize the map below from earlier in the series. It shows the way in which poliomyelitis cases arrayed themselves in 1916 near the Bush Terminal docks. The three-sided rectangle to the left center is the American-Hawaiian dock. We’ll pick it up from there next week.

--
11.
The bulk of the raw sugar headed for the East Coast from Hawaii’s Olaa Plantation left the port of Hilo in February and arrived a few weeks later in New York Harbor. The freighters docked at the American-Hawaiian Steamship Company pier at the Bush Terminal in Brooklyn; as I outlined last week, this is right where many of the early cases of polio clustered. (The dots are polio cases as of July 30; the dock is at the middle left.)
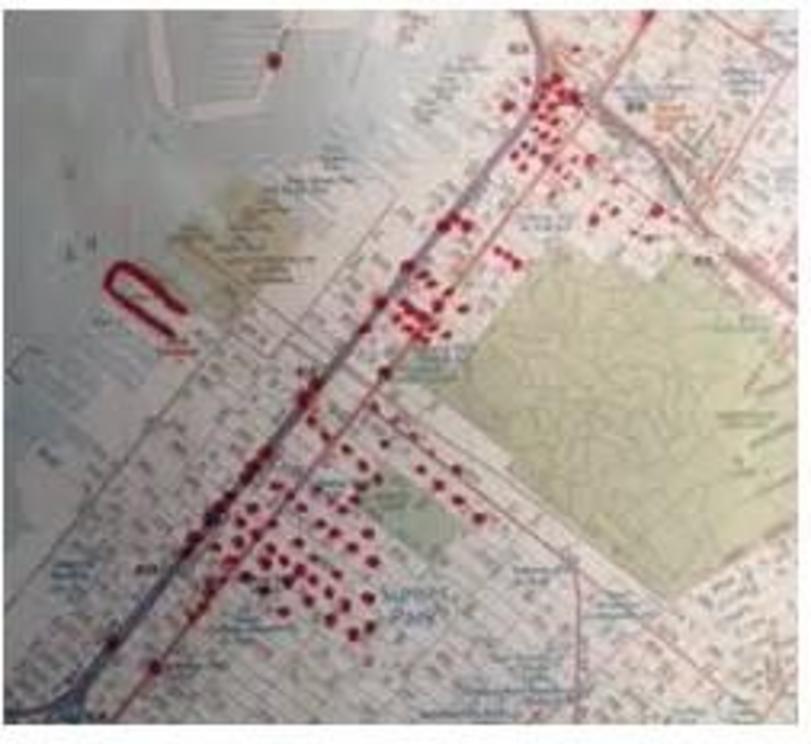
You can see the dock close up below; it’s at the bottom, Pier 7, the one that looks like a tuning fork. You'd have to rotate the image about 120 degrees to the left to align with the map above -- the Bush Terminal piers jut northeast from Brooklyn into New York's Upper Bay.
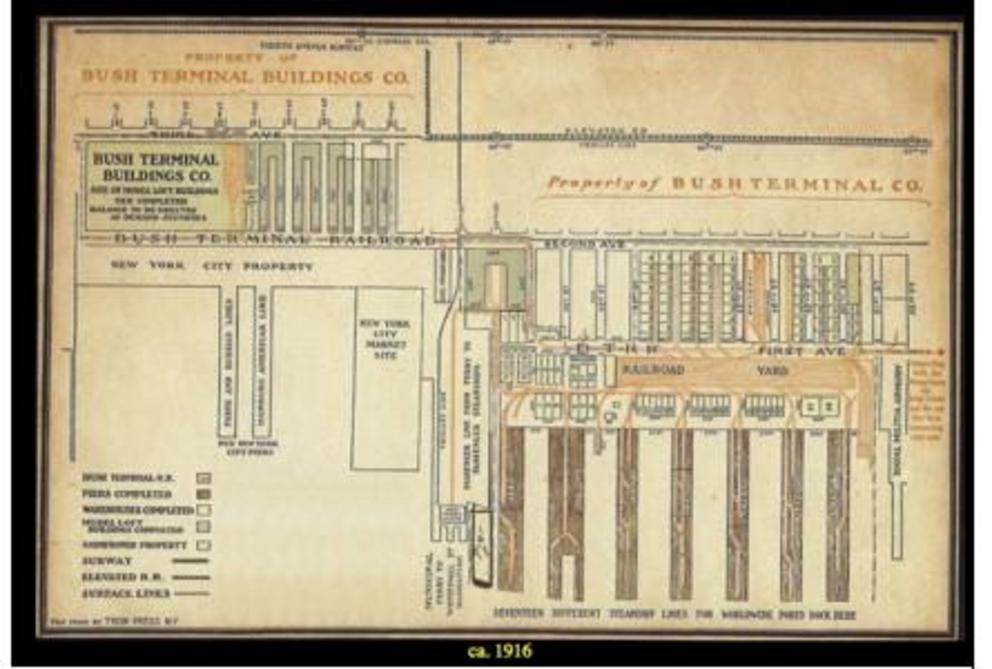
From there the sugar was distributed mainly to the National Sugar Refinery in Long Island City, Queens – at one time the largest in the world -- just across Newtown Creek from Brooklyn,
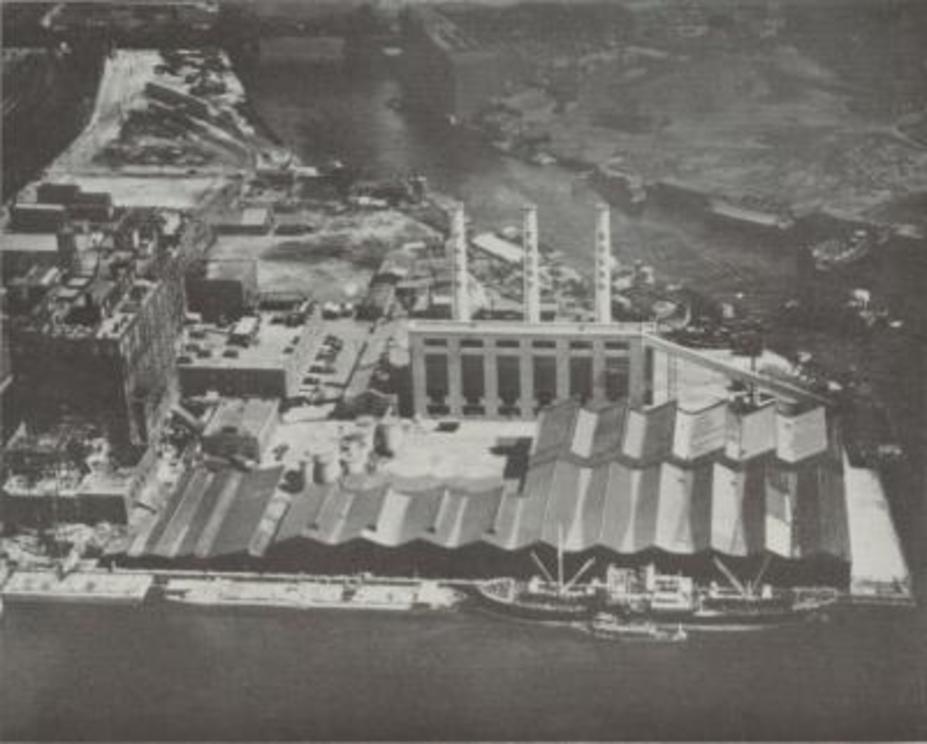
and to a lesser extent to another National Refinery on the waterfront in Yonkers.
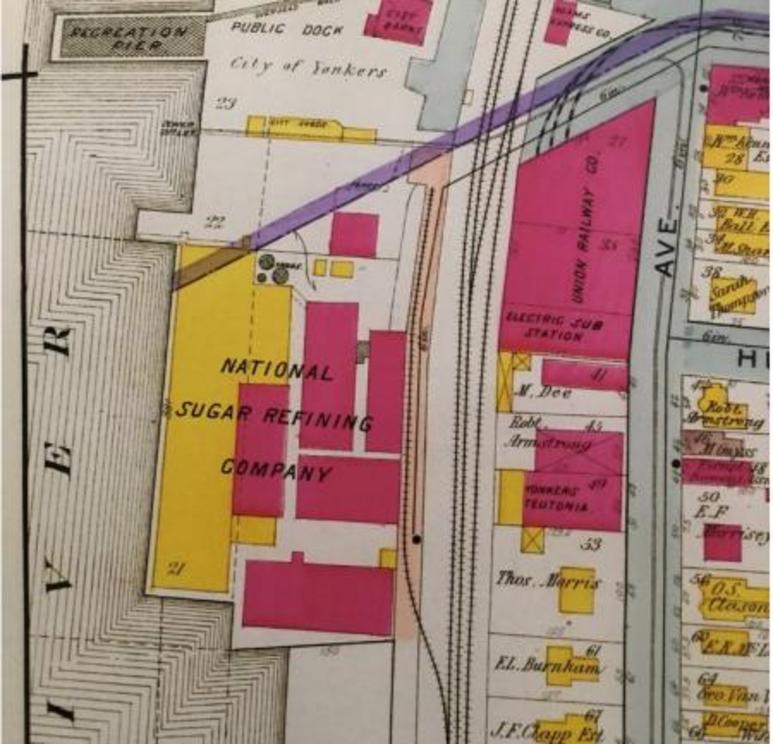
Today the Newtown Creek site is a park awaiting development; the Yonkers plant is still there. A significant amount of Hawaiian raw sugar was delivered separately to Philadelphia, and a smaller portion of it went to Boston. Some stayed on the West Coast at a Hawaiian-owned refinery in Crockett, California.
At the plants, the raw sugar was refined into the finished product. You would think – I did, anyway – that in the ordinary course of events any toxins would be refined away, the refined sugar would be tested for any and all impurities, and once ratified would be on its merry way without any record left behind. Sugar from all over the Western Hemisphere poured through these refineries every day, after all. New York was the sugar refining capital of the world. Hawaiian sugar was just a small fraction of it, and Olaa's was about five percent of that.
But it turns out Hawaiian sugar, and only Hawaiian sugar, gave the refiners fits in 1916. The grains were uneven and too small; “scale” – residue – on the coils in the vacuum pans had to be boiled out with corroded lead every two weeks; the cotton bags themselves tore easily and couldn't be reused. (You can imagine some Hawaiian plantation owner slamming his desk and saying, Dammit, can’t we even get the bags right?) And that was the small stuff. The big issue was there was something in the sugar that they couldn’t get out.
We know this because things got so bad for Hawaiian sugar’s reputation with the refineries that the next year, the sugar producers sent a representative, R.S. Norris, to New York and Philadelphia. (He was dispatched by H.P. Agee, director of the Hawaiian Sugar Planters Association. Agee, as it happens, was the first to suggest arsenic as a pesticide for weeds in sugarcane fields. Agee had succeeded C.F. Eckart, now the head of Olaa and the architect of the arsenic treatment. Small world.)
Norris produced a remarkable report, which was picked up and reprinted as a three-part series (perhaps with more than a trace amount of competitive glee) by the Louisiana Planter and Sugar Manufacturer weekly in February 1918. Two of those problems were pretty striking – first, there was “cloudiness and sediment” in the barrel syrups, liquid created during the refining process that was sold on its own under names like Golden Syrup.
Second, whatever "it" was wasn’t just in the syrup – it was in the grain. At the Yonkers plant,
You can dig a lot deeper into these primary documents – and please do, your thoughts are invited -- but for our purposes right now the point is this: Something in the grain “caused the trouble.” We're no longer talking the weeds or the stalk or the soil or the bagasse. This is the part people consume. I asked the environmental toxicologist who is advising me what she thought: “The article in Planter and Sugar Manufacturer indicates the Hawaiian sugar continued to give off residue even after repeat washing and flocculation with phosphate,” she told me. “They refer to ‘dull gray’ sugar, which I assume indicates that the final product still wasn’t completely purified. There is a discussion at the end of p. 44 about the Hawaiian sugars being ‘polarizing’ due to proportions of glucose and sucrose, which would have enhanced the retention of a highly water-soluble substance such as inorganic arsenic.” It got so bad they had to discount it.
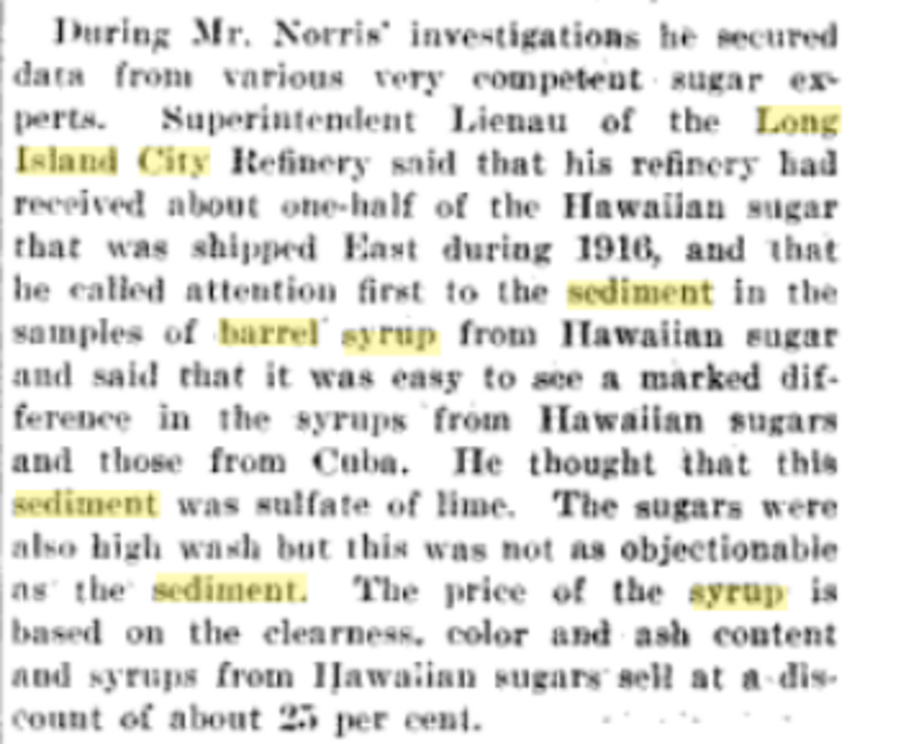
I wonder how consumers would have felt if they knew their kid's ice cream cone for winning the Little League game was made with syrup with so much unknown "sediment" that the vendor got 25 percent off. In Philadelphia it was even worse -- Hawaiian barrel syrup sold for 9 to 10 cents a gallon, Cuban for 15 to 17 cents.
According to my toxicologist: “I read through the brochure on sugar refining that you attached. I see that the sugar syrup is run through a carbon filtration system to remove impurities. This is an issue similar to removing arsenic from groundwater, which is not easy. In the arsenite form, arsenic would tend to run through the carbon filter rather than adsorbing onto the carbon surfaces. On the other hand if the plant has transformed arsenite to arsenate (i.e. added more oxygens) then the carbon filter could probably remove it from the syrup.”
She included several scientific papers for reference. “The Brazilian paper and the German paper both state that the form found in green plants is predominantly arsenite,” she continued. “Thus it’s reasonable to assume that if there was arsenite in the original plants, a good proportion of it would survive the refining process and be incorporated into the crystallized sugar.” There is no mention of arsenic in the follow-up report; one wonders if the possibility had occurred to Agee and Eckart, the two men who pioneered it.
I figured the arsenic, if there was any, would be spun off into barrel or golden syrup, molasses, etcetera. . But my helpful toxicologist wrote: “Scroll down this link until you see the green crystallized sugar. Crystallized sugar can certainly contain other substances. The goal of the refining process wasn’t to remove everything except the sugar molecule; rather the purpose was to extract sugar out of the whole plant. Remember the mention of the ‘grey’ final product? The sugar, let alone the syrups and molasses, would have still contained impurities at the end of the refining process. … More of the impurities remained in the syrup than the crystals, but there would have been some in the crystals too.”
(Norris looked into the sediment's impurities, taking a sample from the West Coast refinery. Here, from the planters' journal, is what he says: "On account of the ease with which the sediment goes into solution and the high density and viscosity of the syrup, we have found it difficult to separate out, and for that reason have not had sufficient time to isolate the substance in a pure form. Analysis of the ash of some of the syrup from which the sediment had been removed and of the crude separated residue showed the main constituents to be as follows" -- then he listed potash, soda, lime, magnesia, sulfuric anhydride and chlorin. After further purification they still ended up with combinations of some of those in the sediment. "The purest product still contains considerable organic matter, so the sediment may be an organic compound. Under the microscope the sediment is seen to be made up of very small, needle-shaped crystals arranged in bundles."
(I asked our trusty environmental toxicologist about this and she replied: "Most likely the crystals were some form of calcium, such as calcium oxide or calcium carbonate. Calcium would have been plentiful in the sediment from the sugar -- note the finding of lime. Arsenic was most likely present but would not have been plentiful in the sediment. On the other hand it didn’t need to be plentiful to be effective. I don’t know the conditions under which inorganic arsenic is converted to the pure crystalline element but no doubt those conditions are more extreme than what is found in a sugar refinery.")
I find it interesting that they didn't have "sufficient time to isolate the substance in a pure form." Really? And also that the sediment "may be an organic compound."
All of this only matters if arsenic made it through the diluting, spraying, weeding, harvesting, milling, and refining and into the final product. The question is how you tell. If there’s anyone who ate spoonfuls of it in 1916 straight out of the bag and got paralyzed, they haven’t left a diary. Barring that, the fact that so many people that year suspected foods that contained a lot of sugar is the most powerful association. Here's a sugar manufacturer describing all the uses to which refined sugar is put:
“Sugar for tea and coffee; sugar for fruits and cereals; sugar for icings, ice-cream and preserving; sugar for candy and chewing gum; sugar for chocolate and condensed milk manufacturers; sugar for cracker and biscuit makers; sugar adapted to an infinite variety of uses, specially made and speedily delivered.”
Now let’s recall the “provision” stores on which suspicion had fallen for the first time that summer of 1916, according to the city’s health commissioner: “There seems to be a well-marked tendency for cases in Manhattan to appear in the immediate vicinity of stables, groceries, meat or poultry markets, lunch rooms, delicatessen shops and bakeries or macaroni factories. … It is surprising with what regularity one or the other is found in the building next door to a house in which poliomyelitis has occurred. Others who have also examined the same districts with an unbiased mind, seem always to believe that cases range themselves with a definite relation to shops of this type. It has been repeatedly pointed out in earlier epidemics that stables are often associated with cases of poliomyelitis. This has been undoubtedly true in New York during the present summer, but the other association with provision shops has also forced itself upon our attention.”
It’s worth deconstructing this crucial paragraph once more. Haven Emerson, the commissioner of the city health department responsible for tracking and slowing the epidemic, considered the “ice cream and candy” idea to be nonsense – as have all the other experts for the past 100 years -- and he submerges it in that paragraph beneath generic “food,” “provisions," and a nearly impenetrable prose style. But as you may recall, Emerson’s report includes a chart linking "provision" stores with clusters of poliomyelitis. And now, with more specificity, another pattern emerges:
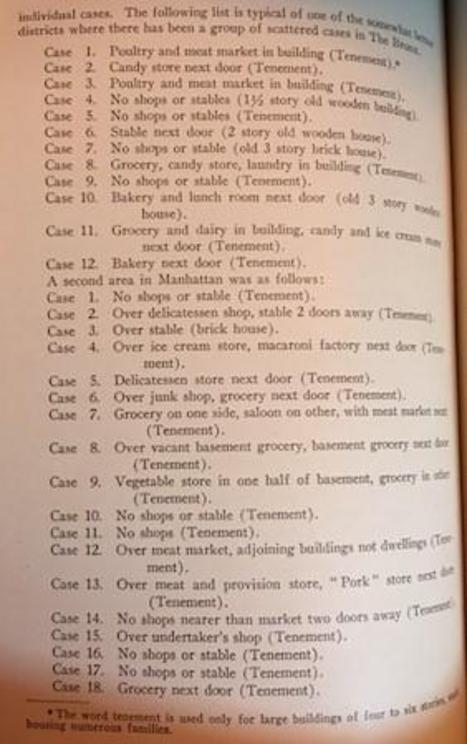
Candy. Grocery. Bakery. Ice cream. Candy. Grocery. Bakery. Ice cream. Candy. Grocery. Delicatessen. Grocery. Lunch Room. Grocery.” That comes just a few pages after Emerson’s dismissive reference to those who wrote letters to the health departments. “Two hundred and thirty suggestions as the cause of the disease were received, the largest number of authors (80) attributing the existing calamity to foods. Ice cream, soft drinks, candy and summer fruits were generally accused, cereals and canned foods coming second in favor.”
So “unbiased” minds who did have the respect of the health department, and letter writers who didn't, saw the same thing: Foods that contained a lot of sugar – the sugar link was unmentioned and perhaps unrecognized – were the chief suspects. How far are we, really, from the companies' own list of “sugar for fruits and cereals; sugar for icings, ice-cream and preserving [canned foods]; sugar for candy and chewing gum; sugar for chocolate and condensed milk manufacturers; sugar for cracker and biscuit makers; sugar adapted to an infinite variety of uses, specially made and speedily delivered?” I’ll go out on a limb and say, not far.
Here are two ads of the era. Domino was another huge Brooklyn sugar refinery; it is not one we’re discussing here, but the uses of “barrel syrup” (golden syrup) are neatly described.

So we've got golden syrup with sediment in it, and grains of sugar with something in them, showing up in 1916 on bread, muffins, fruit, fritters and ice cream, waffles, griddle cakes and fried mush, and in cookies, cakes, muffins, puddings, sauces and baked beans. And much else. Here’s an ad from a condensed milk manufacturer. Despite its wholesome name, anyone who has ever scooped a spoonful knows it's half sugar. Here it is rather unashamedly marketed toward mothers of infants (that’s a condensed milk can with a spoon for each child):
Before we finish, it's worth inserting a number of caveats. As I said, I don't know exactly where all the Olaa sugar went. Some may have gone to the refinery in California, where there was no poliomyelitis epidemic, which does nothing to advance the theory. Furthermore, there's no direct evidence of arsenic in refined sugar anywhere at all in 1916. Just because arsenic was used to kill weeds on a Hawaiian sugarcane plantation for the first time in 1916, and there were issues with the quality of Hawaiian sugar in 1916, and it was refined at the epicenter of the epidemic just before the outbreak, doesn't mean the outbreak had anything to do with arsenic.
It might have been arsenic in sugar, but not from Hawaiian pesticide treatment. In 1900, there was an outbreak of arsenic poisoning in beer tainted by sugar that had been manufactured with sulphuric acid containing arsenic. Authorities first thought the subsequent illnesses came from drinking too much -- another case of blaming the victim.
It might have been sugar -- but as a vehicle for the virus, not the arsenic. Perhaps the virus finds sugar hospitable -- the sugar cubes used to deliver the live-virus vaccine must mean it does. The whole epidemic could be illustrative of nothing more than the wisdom of the ubiquitous restroom sign, "Employees must wash hands before returning to work."
Or maybe it's just the sugar, nothing to do with either the virus or the toxin. We've been discussing that in the comments, whether sugar consumption itself makes one more vulnerable to paralytic illness. That is the strong form of the "sugar and diet" argument.
David Burd sent me this interesting article from 1991 connecting the ebbs and flows of the sugar growing and refining business -- including sugar beets, a whole vast area that I haven't touched on -- with poliomyelitis epidemics.
https://www.vaccinationcouncil.org/wp-content/uploads/2013/08/diet-and-polio-Van-Meer-science.pdf
My problem with this is it works almost too well, explaining everything that ever happened in terms of sugar. It's easy to put yourself in a box if you make too many claims for one source of causation, and blind yourself when it manifests in new ways.
So I've stuck to 1916 in this series, and to one basic hypothesis I've put to as many tests as possible. And despite the caveats and the unorthodox novelty of the idea, I find the evidence intriguing -- a toxic metal was first used on sugar shipped to New York Harbor right before the first big poliomyelitis epidemic broke out there. Families living near the dock where it was delivered suffered the first cases. There was widespread suspicion that summer of a variety of foods whose only apparent commonality was that they contained a lot of sugar. Plus it's biologically plausible -- both the virus and arsenic end up in the gut where "amplification" could turn a common and harmless enterovirus into a deadly and damaging epidemic. It explains the anomalies of a paradigm -- the hygiene hypothesis -- that doesn't really fit the facts.
That brings us full circle, with Mrs. Franklin collapsing paralyzed in June in her ice cream store in the tenement on Gates Avenue in Brooklyn, a place where two infants, one living in the apartment adjacent to the parlor, had recently died. Here's what I think: The Age of Polio, and of subsequent modern epidemics like autism, had just exploded into view. Sadly, there was so much more to come.
12.
When Mrs. G.H. Franklin woke up after collapsing on the floor of her Brooklyn ice cream parlor on June 19, 1916, she found herself in a ward at St. Mary’s Hospital, paralyzed. She was 56 years old. Just two days earlier, the Brooklyn Daily Eagle ran a story on its front page headlined “24 Cases of Infant Paralysis in the Boro; Health Board Acts.”
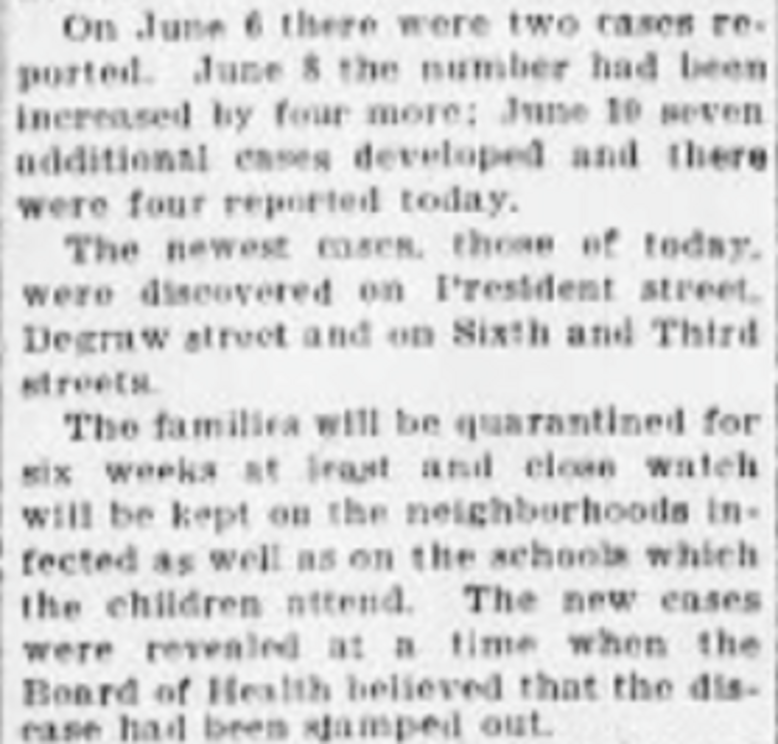
Despite the timing, doctors were loathe to describe Mrs. Franklin's case as polio. For one thing she simply seemed too old for infantile paralysis -- the oldest person in the health department case files that summer. “The hospital records show that the case was considered some type of meningitis altho a lumbar puncture showed nothing abnormal,” according to a health department report. “On July 8 she was brought to her son’s home at 1250 Curtis Avenue, Woodhaven, Queens. On July 30, after she left, her grandsons Herbert and Calvin were taken acutely ill, the former promptly being diagnosed poliomyelitis, the diagnosis in the latter not yet known. “On July 15, Mrs. Franklin moved to 4559 Metropolis Avenue, Queens, and nine days after arriving there, her grandson Willy was taken ill and also Edith Smith, the daughter of another tenant in the same house. Both proved to have poliomyelitis.
“An interesting sidelight on this problem is the fact that on June 1, when Mrs. Franklin was first taken ill at 1295 Gates Avenue, an Italian baby on the top floor became suddenly ill and died within 24 hours, no diagnosis being made.” Trying to untangle the coincidences from the clues was beyond the health department’s ken. Yet the department spent a lot of its time building up voluminous files on each case and tracking down every possible contact. This was a misadventure if the hypothesis I've laid out in earlier segments is true, because it continually missed the environmental trigger -- low levels of arsenic in sugar that had recently arrived at the refineries from Hawaii.
The environmental toxicologist who’s been helping me commented: “Arsenic in sugar would result in intermittent dosing, which is more likely to manifest in some of the other known symptoms of arsenic toxicity such as GI upset. Orally ingested arsenic is very hard on the intestines. Orally ingested poliovirus enters the body through the intestines, which will be less able to fight off a viral invasion if arsenic-induced inflammation and necrosis is present.” Certainly plenty of polio cases I’ve read about from the 1916 epidemic began with that kind of stomach upset. I wonder if Mrs. Franklin got better just because she was no longer eating her own ice cream all day.
--
Brooklyn, where the Hawaiian sugar made port, had the first outbreak. Queens, where most of the raw sugar went to the refinery in Long Island City, had the highest polio rate per capita of the five boroughs. Yonkers, where a smaller amount went to the refinery there, had the highest number of cases of any city of its size in the country. That’s proof of nothing but it’s consistent with the “facts cluster around a good hypothesis” model.
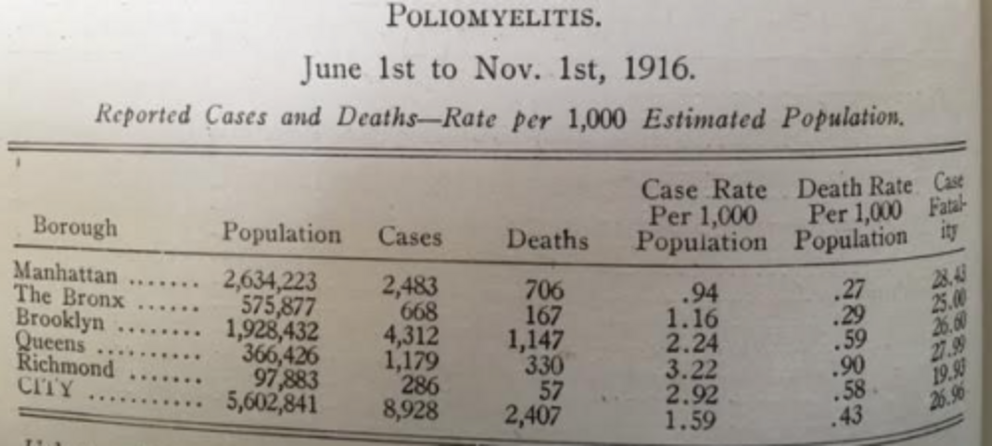
More clues, also direct from the health department:
Here is that cluster on the health department’s map – it’s directly opposite the green square:
The refinery itself is marked in dark blue, cut off by the railroad tracks, the East River and Newtown Creek. The neighborhood described above was as close as you could get to the refinery without setting up your home on the railroad tracks. (For reference that’s Roosevelt Island at the top.) Here is the Long Island City refinery (the blue dot), also once the world’s largest. You can see how the complex is bounded by the river, the creek and the railroad tracks. The cluster of houses with polio cases was to the immediate left.
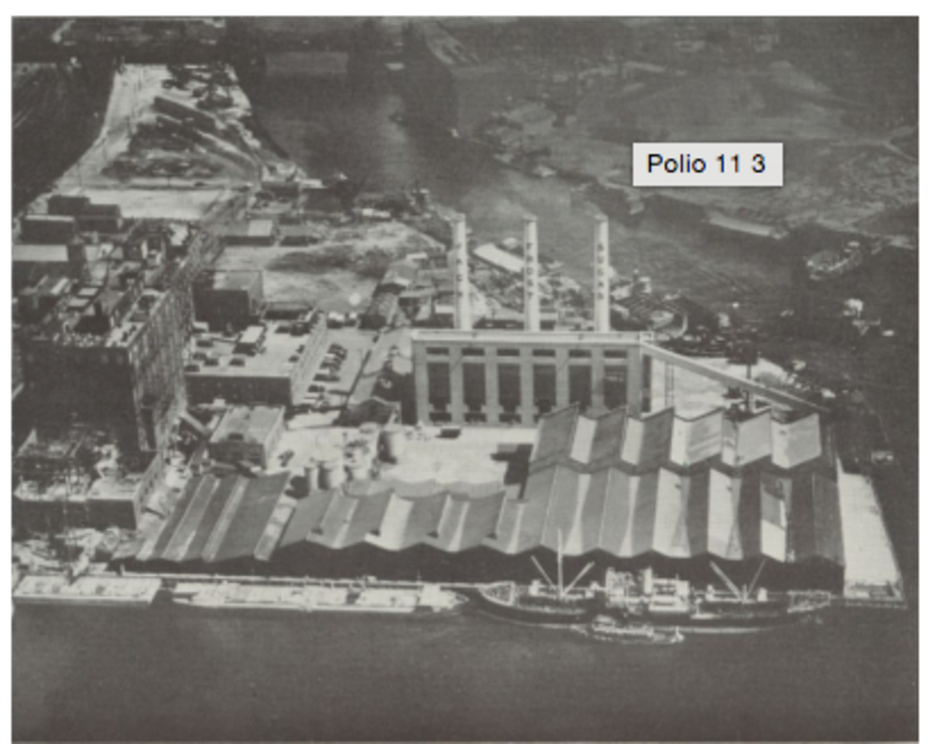
In the health department's contact-tracing files now archived at the American Philosophical Society in Philadelphia, I came across a man who worked at the Long Island City refinery..
--
Dept of Health
City of New York
Memorandum for Dr. J.S. Billings, Deputy Commissioner of Health, August 28, 1916
Food
Borough of Brooklyn
Maddie Violetta – Poliomyelitis
127 Eagle Street – first floor, front
Father works in sugar factory
9.1.16 Insp. Jones investigated above case and reports as follows. Patient treated at home. Another child 4 years also at home. Father Michael Violetta employed by the National Sugar Refinery Co., Front St. Long Island City. Interviewed father and instructed him to live away from home, or discontinue work. He stated he would stay at 44 Bradley Ave., Blissville, L.I., until recovery of child and completion of renovation. Will keep under observation.
--
Another reference to Long Island City comes from the most affecting article about polio I’ve ever read, by a nurse named Charlotte Talley in the November 1916 issue of the American Journal of Nursing. Despite its clinical title, “Tracing the Sources and Limiting the Spread of Infantile Paralysis: Second Paper,” it is heartbreaking:
“’Blease, blease, do something,’ pleaded a Polish mother hysterically, clasping her hands in supplication, her mouth quivering. ‘They took my boy to ‘ospital and see,’ showing the bathtub full of soiled clothing, ‘here are all the clothes from the sickness and no water to wash ‘em. Landlady said she get plumber today. She gets no one.’”
Such scenes of desperation flooded the city.
“A little girl of nine had died of paralysis after a few days of great suffering. She had been a beautiful, bright, lovable child, the pride of the household,” Talley wrote. “Apparently, despite all her parents’ precautions, she had played with a neighbor child with an inapparent infection and may have been exposed to the virus that way.”
Talley shows us why polio came to be so feared -- crippling, deadly, often agonizing and utterly unpredictable -- though its prevalence was never as high as other horrible childhood diseases. And she offers two more relevant stories. In one, a Long Island City food store was forced to shut down.
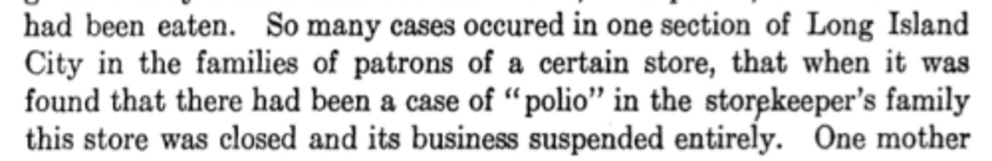
This is what "unbiased minds" around New York City had been reporting -- cases clustering around various food emporiums. In this case it was right next door to the sugar factory. Then there is this remarkable vignette which needs to be read in full:
Isn't this practically a field test of the sugar hypothesis? Five children more or less isolated, eating only garden vegetables … and foods with a lot of sugar. Condensed milk is just about half sugar. Let’s look again at the contemporary advertisement of four babies with their spoons, set to devour a can of condensed milk:
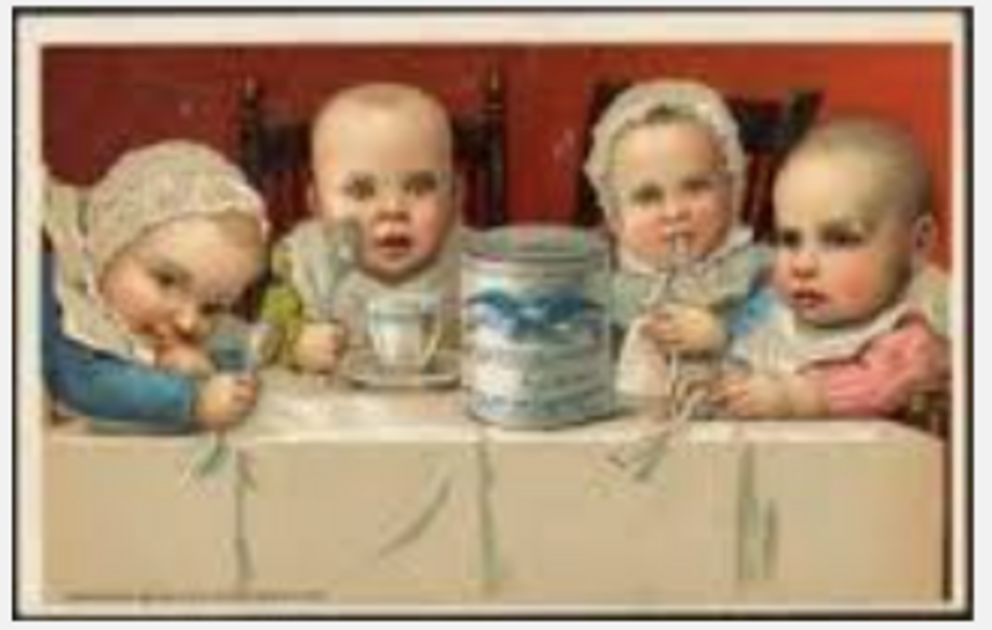
--
Yonkers was the other place in New York that Hawaiian sugar went. And it had the highest rate by far of polio for any city of its seize. Of course, it’s also closer to the center of the epidemic, Brooklyn, than many other places. But check out this list, which puts Yonkers far ahead of most other cities, including close-in ones like Bayonne and Hoboken.
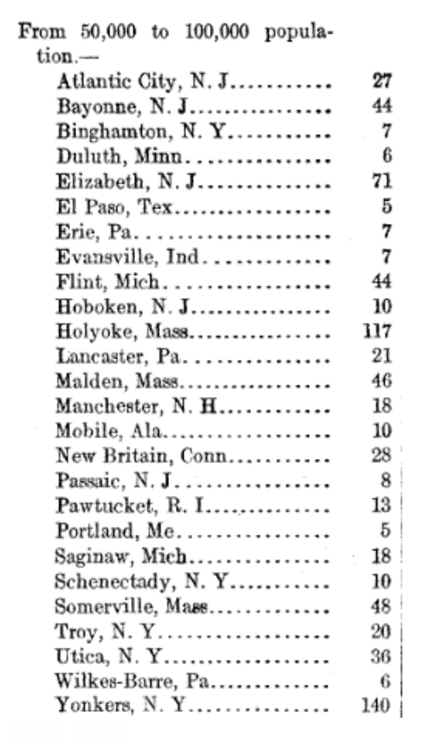
AOA Contributor Lou Conte grew up in Yonkers and recalls ships offloading sugar along the East River. “You could smell the sugar in the air. It was incredibly messy process and it was obvious that some of the sugar powder became airborne.”
--
So the facts, and the polio cases, continued to cluster around the sugar-arsenic hypothesis. Interacting in people, mostly children, with active polio infections, a "light" arsenic exposure turned a benign summer bug into a poliomyelitis epidemic. We see the evidence in the way the early cases clustered around the Brooklyn port where the sugar arrived; we see it in Queens and Yonkers, with the two sugar refineries and the highest proportion of cases. We see it in the kinds of foods that ordinary people came to suspect; we see it in the health department's own list of "provision" stores around which cases repeatedly clustered, notably in Long Island City. We see it in the remarkable story of four out of five children in one isolated family.
And we see it in baffling sagas like Mrs. Franklin's. By early August, she was “able to get up and walk around, but when I saw her today she had a temperature of 100 2/3 and has not good use of her arms yet,” the public health worker said. “She has been attended by nine different physicians in the past 2.5 months. All diagnosed her case differently, but the last said she had a light case of meningitis." Which matches a "light" case of arsenic exposure.
As the epidemic began spreading beyond the confines of New York’s five boroughs, that diagnosis was about to change as well.
13.
In this series I’ve proposed that the polio epidemic of 1916, which started in Brooklyn and spread to all five New York City boroughs and finally the entire Northeast, was triggered by arsenic, used for the first time ever, as a weed killer on one Hawaiian sugar plantation. The sugar that I suspect was arsenic tainted arrived by freighter at the Brooklyn docks, was unloaded and then refined at mammoth factories in Queens and Yonkers, and ingested by children who also were exposed to the poliovirus, triggering the first big regional poliomyelitis epidemic.
On the face of it, the notion seems too complicated and unlikely to make sense, a kind of Rube Goldberg version of a simple mousetrap involving chutes and ladders and bells and whistles rather than a coiled spring and a piece of cheese. Isn't polio just a viral infection that in some unlucky cases causes paralysis and death? (Or isn't it just a toxic injury passed off as a virus, as some readers believe?) My answer is that it's an interaction of the two. It's what makes that small percentage of children "unlucky." As I quote Einstein at the start of the series, "Everything should be made as simple as possible, but not simpler." Nature in this case has not provided a simpler explanation, which may make it harder to accept but has no bearing on whether it is true or not.
But why bother, at this late date when polio has been eliminated in the U.S. and nearly wiped off the face of the Earth? Well, for one thing, it's endlessly fascinating as a medical and cultural saga that continues to misinform our understanding of disease and how to prevent it -- the fear of iron lungs has led to a phobia of even the most benign of childhood illnesses and the cult of vaccination uber alles. Most important, it is the same kind of mechanism that I believe has led us into the Age of Autism -- live viruses whose harm is "amplified" by the presence of toxic metals like mercury and aluminum. Autism is a man-made epidemic. So is polio.
By taking on polio, I'm laying the groundwork to understand and accept the same mechanism in autism and other modern illnesses. Ultimately this series has as much to do with Michelle Cedillo and the 5,000 other children in the Omnibus Autism Proceeding as it does with the 2,500 children who died in New York City that summer of 1916. False narratives need to be taken down and replaced with the truth, and it's never too late.
--
One hundred years ago the ability to detect and remove minute quantities of a toxin like arsenic from a substance like raw sugar would have been lacking. That's according to an AOA reader and environmental toxicologist who has been helping me understand the chemistry behind this idea. This week I asked her if white arsenic -- the type of arsenic used on the Hawaii plantation, Olaa, as a pesticide -- would have been harder to detect because it looks like sugar.
Her response: "The relevant characteristic is not what arsenic trioxide [white arsenic] looks like when dried, but how it behaves when in solution. Both sugar and arsenic trioxide dissolve readily in water and they can’t be separated out from the water with the types of filtration systems used in a sugar refinery 100 years ago. Those passive filtration systems were designed to catch larger types of molecules, including parts from crushed plants, crushed dirt/stones, crushed insects, etc.
"Arsenic trioxide, or arsenite, has a very strong attraction to the water molecules, so you have to use an active system like reverse osmosis to separate it from water. Sugar and arsenite would 'travel together' all the way through the filtration process; the final product, when dried, was just white crystals so there would have been no visual clue that arsenite was mixed in with the sugar."
She also explained: “Arsenic in sugar would result in intermittent dosing, which is more likely to manifest in some of the other known symptoms of arsenic toxicity such as GI upset. Orally ingested arsenic is very hard on the intestines. Orally ingested poliovirus enters the body through the intestines, which will be less able to fight off a viral invasion if arsenic-induced inflammation and necrosis is present.”
--
So far we’ve traced the roots and rise of the 1916 epidemic from Brooklyn through the rest of New York City, including Queens and Yonkers which had the highest rates of polio of the five boroughs and of any city with a population between 50,000 and 100,000, respectively. Now let’s look at the big picture and see if the correlations continue. In an interesting 2011 medical journal article, H.V. Wyatt suggests the virus must have mutated (and then escaped from a lab in New York City) in order to explain the unusual characteristics of the epidemic:
--
All this argued that something unusual was going on, whatever one’s theory of the case. In the first article in the series, I wrote: “What set off the Explosion of 1916? If I'm right, an environmental bomb landing in just about the worst possible place at the worst possible time set it off, the impact spreading with a smooth but terrible precision like ripples from a pebble dropped into a still volcanic lake.” That was an allusion to the evidence that would follow linking it to Hawaiian sugar.
Here is the U.S. Public Health Bulletin in 1918 describing the way the epidemic rippled throughout the Northeast and adjoining areas:
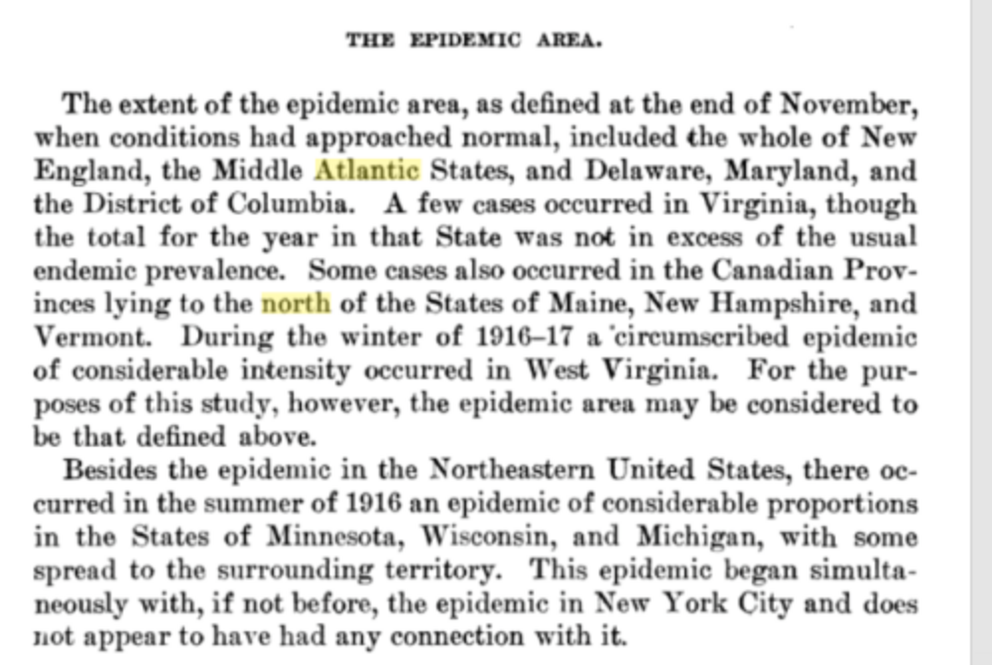
Here’s how that looked in the Northeast county by county (Pennsylvania didn’t report statistics so you have to imagine a blotchy pattern of cases there as well):
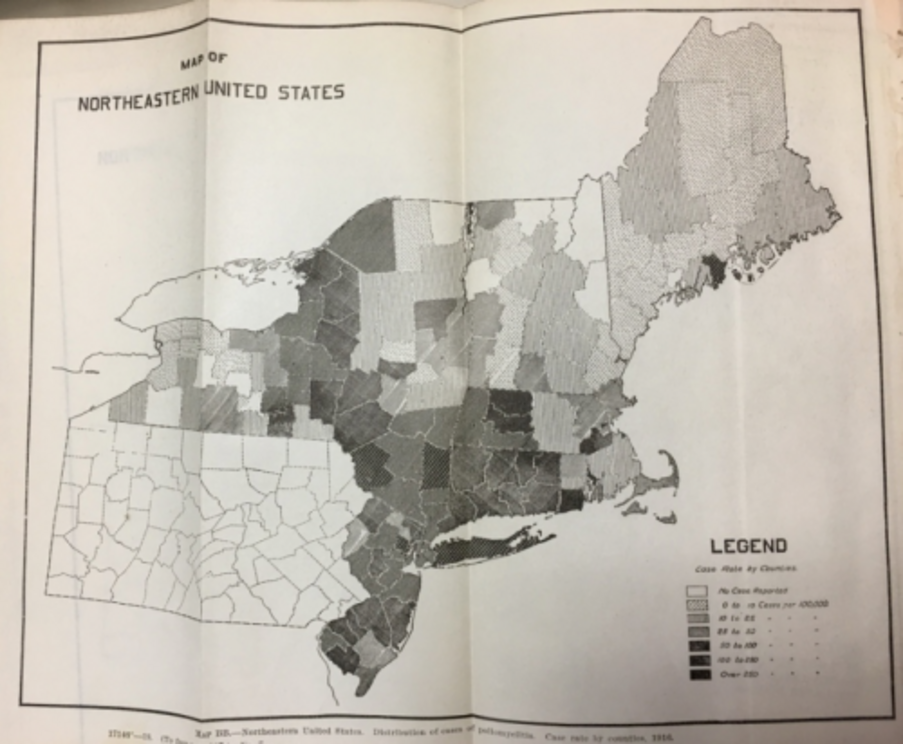
And here’s how it looked in terms of actual cases:
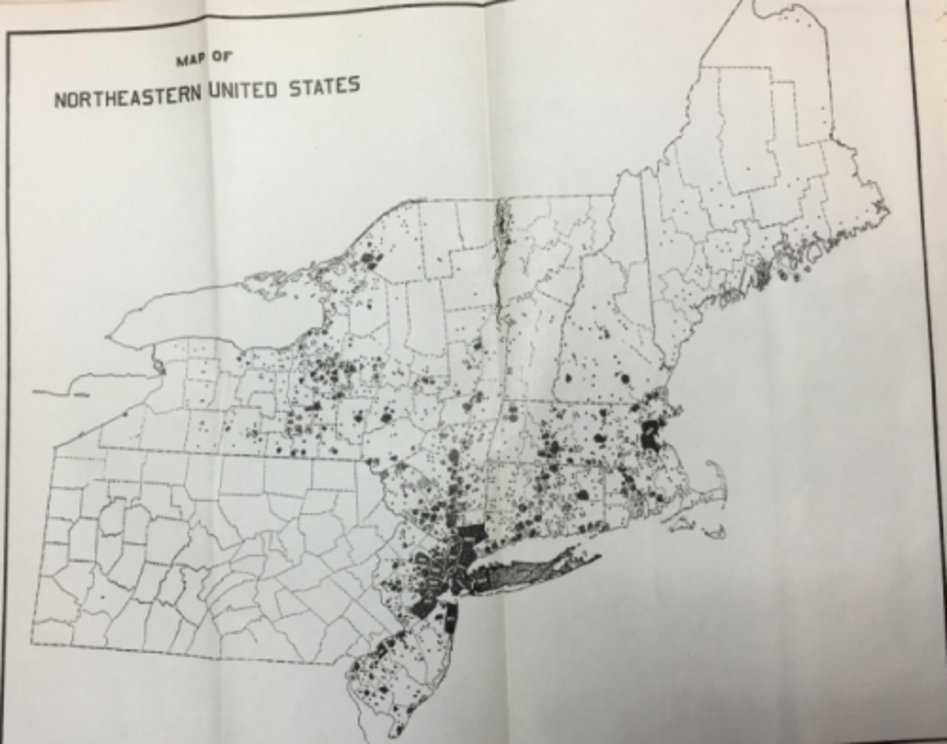
And here’s one more way of looking at it:
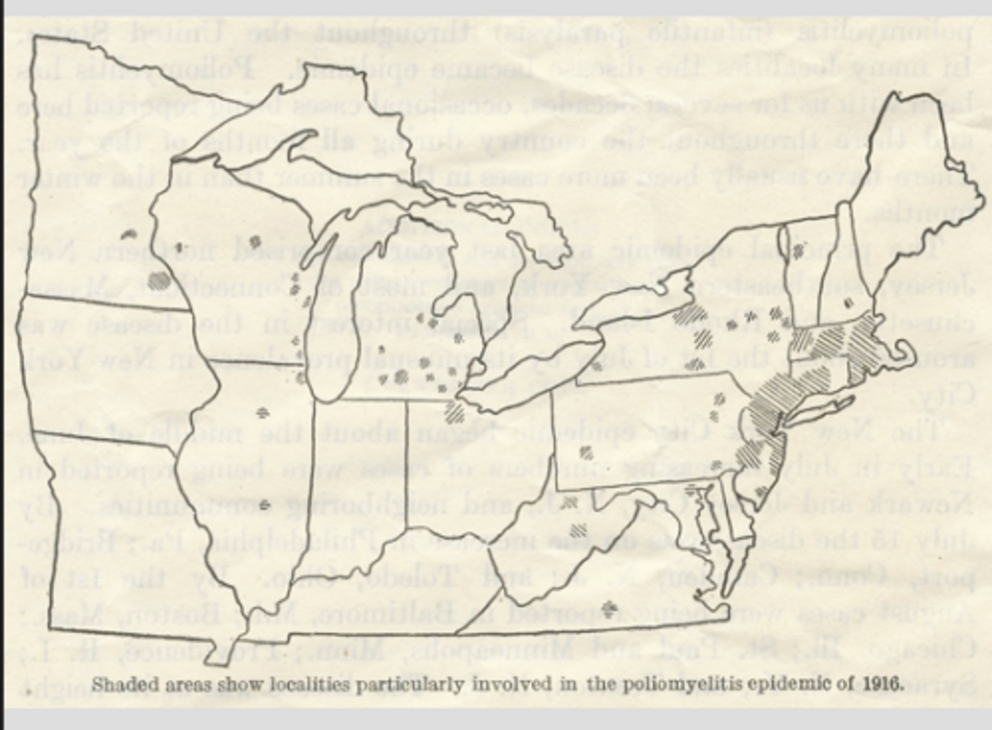
Finally, let’s compare this to sugar distribution in 1916. As I’ve outlined, the bulk of Hawaiian sugar arrived in New York Harbor and Philadelphia early in 1916, while a lesser amount to Boston. (Some also went to the refinery in Crockett, California.) Some sugar cane – but not from Hawaii – was processed in Charleston, another East Coast port that received raw sugar from Cuba and Puerto Rico, and also in Louisiana, which grew and refined its own. Then there was the huge crop of sugar beets, grown and processed in the heartland and western states.
Here are sugar distribution zones from a 1959 government publication. The Northeast, the Middle Atlantic, Maryland, Delaware, Washington, D.C., Virginia, West Virginia, Michigan and surrounding states -- this looks like the territory of the polio epidemic to me.
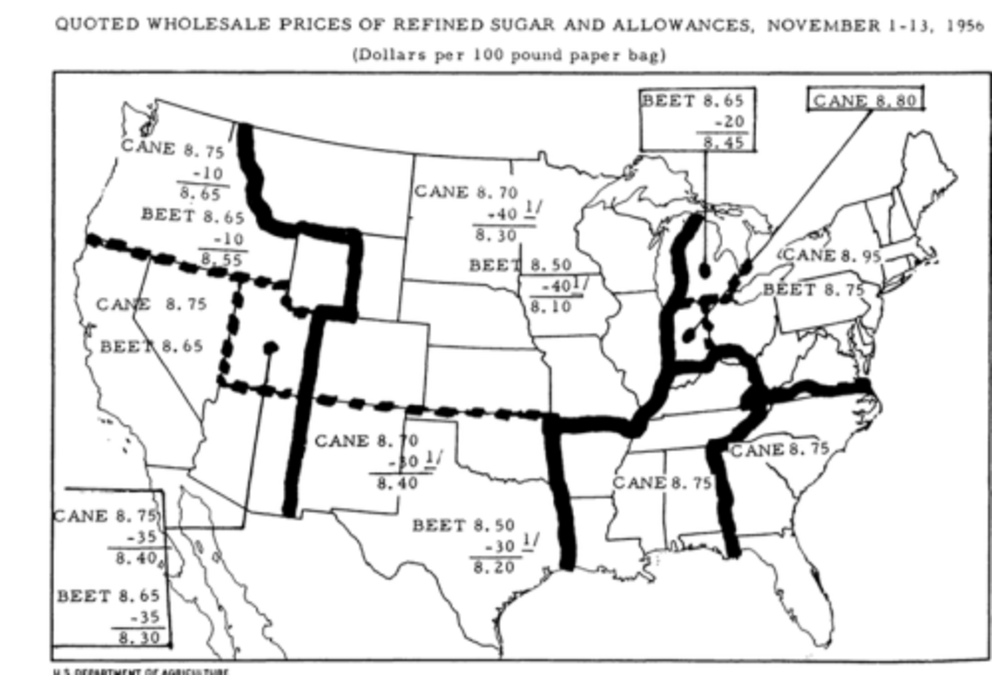
I couldn’t find a distribution map from 1916 (f anyone can, please let me know), but a couple of years after the 1916 outbreak, when sugar rationing went into effect in the United States due to World War I, here is how the sugar board divided things up:
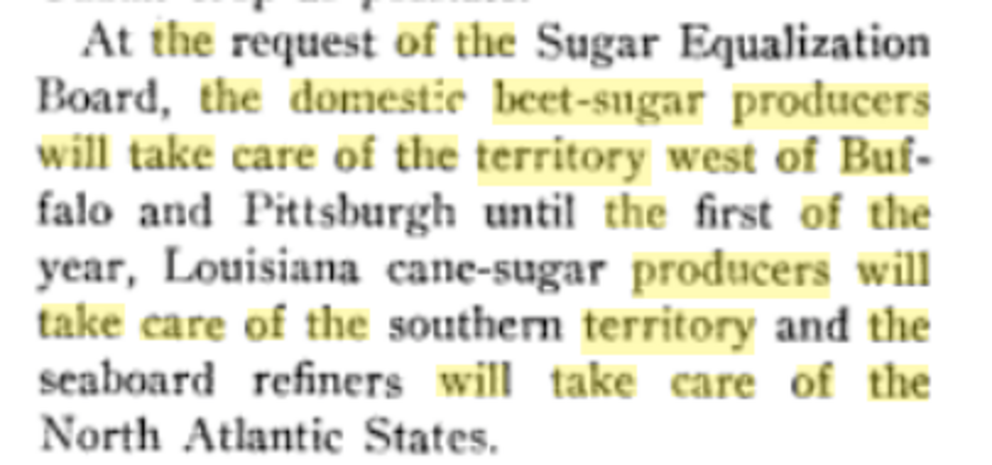
That suggests the sugar was distributed about how you’d expect, along regional lines closest to the sources of production. The North Atlantic States pretty much match the hardest-hit 1916 poliomyelitis outbreak states.

I’m well aware correlation does not equal causation, and that the evidence presented in this series so far is not dispositive -- that's why future installments will delve into other outbreaks to lay down as much evidence as I possibly can. Nonetheless, a look at the big picture of Hawaiian sugar refining and distribution from New York, Philadelphia and Boston in 1916 does nothing to falsify the idea presented in this series so far. Facts, as my colleague Mark Blaxill says, cluster around a good hypothesis. I also admire the words of Judge Francis Buller to the jury in a 1781 murder trial, which we quoted in our book The Age of Autism:
“You are not to expect visible proofs in a work of darkness. You are to collect the truth from circumstances, and little collateral facts, which taken singly afford no proof, yet put together, so tally with, and confirm each other, that they are as strong and convincing evidence, as facts that appear in the broad face of the day."
--
The circumstances, the collateral facts, and the evidence do seem to connect and confirm each other. As I’ve shown, the “experts” lampooned and failed to follow up on repeated observations that sugar-heavy foods, from candy to baked goods to soft drinks to the places that sold and served them from Coney Island to grocery stores to delis and lunchrooms, seemed to be the centers of polio outbreaks. That dismissive approach by the "experts" to eyewitnesses and "ordinary" people is an ongoing tragedy and an overriding theme of this project. Just because they failed to take it seriously a century ago does not mean we can't take it seriously now. That's what historical epidemiology is all about.
Let’s end our survey of the New York epidemic where we started, with the widely lampooned idea that “ice cream causes polio,” a supposed classic of false correlation, even though people cited it repeatedly at the time. That brings us back to Mrs. G.W. Franklin and her ice cream store at 1295 Gates Avenue in Brooklyn, the one “all the children naturally frequently,” in a building where two cousins died in May 1916. It’s the place where Mrs. Franklin collapsed on the floor on June 19, paralyzed. It was a strange scenario that matched the observations people were making about places like that being the center of polio clusters. Yet the public health commissioner at the time, Haven Emerson, said: “It may not add to the sum of scientific data to quote the suggestions received by the Department of Health as to the cause and means of curing or preventing poliomyelitis; but as a record of human interest the letters sent from all over this country and from many foreign lands present a picture which it is well for health officers to bear in mind. One hardly knows whether to laugh at the fantasies or weep over the ignorance and superstition exhibited. ...
“Two hundred and thirty suggestions as the cause of the disease were received," he continued, "the largest number of authors (80) attributing the existing calamity to foods. Ice cream, soft drinks, candy and summer fruits were generally accused, cereals and canned foods coming second in favor."
We recounted Mrs. Frankin's journey to the hospital and then her release and recovery to the point where she could walk again. Nine different doctors treated her, unsure of what she had, settling on “a light case of meningitis.” In an undated report by a health department nurse she is described as “able to be up and around and shows no sign of paralysis although she is still very weak.” By then the diagnosis had changed, too. “There can be no doubt that Mrs. Franklin had poliomyelitis and as far as our records go this is the oldest case on record.” She was 56, strikingly old (in fact, the oldest) to come down with the illness for the first time, especially surrounded by children for years.
It was not, sadly, the final note in the file. From a card dated October 6, just as the first great epidemic that presaged the next 40 years of disability and death and terror was beginning to burn itself out:
“Name of patient: Mrs. G.W. Franklin.
“Patient was taken to Jamaica Hospital about September 20 and died October 1. She never entirely regained use of her limbs.”
--
14.
The first articles in this series told the story of the 1916 polio epidemic in New York City and the North Atlantic States. I put forward a theory that arsenic, used for the first time as a pesticide on a Hawaiian sugarcane plantation, got into the sugar supply in the refineries in New York as well as Boston and Philadelphia. The arsenic interacted with the poliovirus -- "amplified" its ability to cause paralysis and death by gaining it access to the nervous system and the anterior horn cells at the top of the spine. That led to the largest polio outbreak up to then, with nearly 2,500 dead in New York City alone.
This is a novel idea, to say the least, and the evidence I presented for it was indirect – above all, the widespread observation by ordinary people that certain foods like ice cream, candy, soft drinks and baked goods, and the places that sold them, were vectors and epicenters of the epidemic. Along with other evidence, these observations pointed, in my mind, to sugar as the common ingredient. I tracked cases from the docks in Brooklyn where raw sugar from Hawaii was unloaded to the refineries in Queens and Yonkers and Boston and Philadelphia where it was processed, to the wider North Atlantic distribution area that mirrored the spread of the epidemic. Public health officials of the day disregarded and even mocked the observations; when more than half of all letter-writers mentioned food, and the list began with ice cream, soft drinks, candy and summer fruit, the New York Health Commissioner said he didn't know "whether to laugh at the fantasies or weep over the ignorance and superstition exhibited." Germ theory was in ascendancy and environmental illness was not even on the radar, which did not exist, either. Two factors as the root of polio epidemics would have seemed fiendishly implausible. Wasn't one more than enough to try to wrap your mind around?
If the arsenic co-factor theory is true, and I certainly believe it is, we ought to be able to apply it to other polio epidemics, whatever the delivery and exposure mechanism. That would be a reasonable and fundamental test. But how do we logically proceed? I can think of four ways. We could look for direct evidence of arsenic in other polio epidemics. We could look for other toxins beside arsenic that could have been co-factors separately or in combination. We could look at sugar and see whether, in subsequent years and places, it emerges once again. Or we could look for signs of an association with food more broadly.
In fact, I'm going to do all that. But for starters, let’s pick food, which is the big clue from the New York epidemic. This week, I happened to come across an account of an outbreak in 1926 while doing other research this at the National Library of Medicine in Bethesda, Maryland. It just popped up, as facts tend to do around a good hypothesis. The article, no more than a page long, concerned a 1926 outbreak in the Broadstairs area of Kent, England.

The article ran in the January 15, 1927, edition of the British Medical Journal.
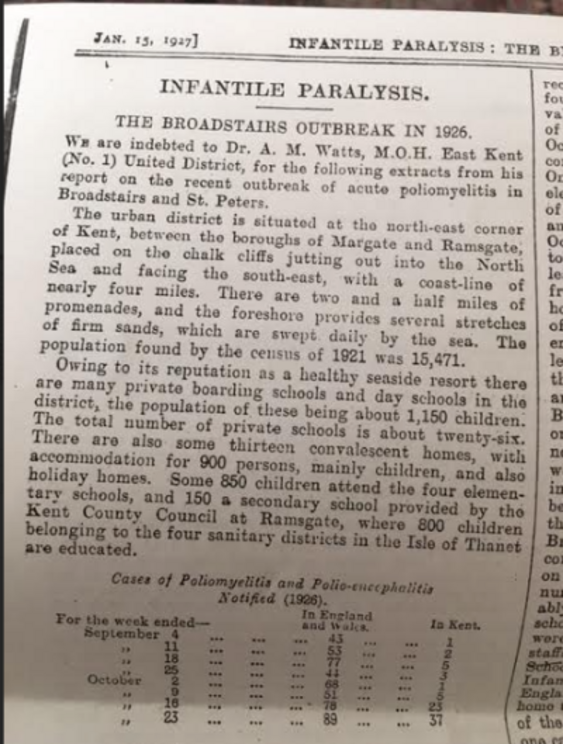
The epidemic began in October and primarily affected children at certain schools in the area. Under “interesting features” of the outbreak were four facts:
- “The disease was limited mainly to the children attending private schools in the district, particularly boarding schools … the private schools had very little communication with each other.”
- “The disease started almost simultaneously in all the schools affected, and ceased almost entirely at the end of a fortnight.”
- “The disease did not spread to the adjoining districts.”
- “The disease did not spread in the elementary schools.”
Out of 67 cases, in fact, “there were 12 … that were not connected with the schools or institutions, except indirectly – for example, one whose brother attended a school where a case occurred.” (That was the only such example given, alas. Having a brother who attended the school seems barely "indirect.") One mistress and two members of domestic staffs at the private schools were also affected. In one convalescent home there were two children and three staff members affected.
“Then,” the report continues, “there was the case of a waiter, aged 22, employed in a hotel in Broadstairs during the season, who left the town on October 6, developed the disease on the 16th, and died in a London hospital on October 21; and that of a young woman, age 29, who stayed in Broadstairs from October 2 to October 9, and died on the 22nd.”
The authors also cite the case “of the brother-in-law of the headmaster of one of the schools, who had been staying in Broadstairs for three weeks. He visited the school on October 10 and had lunch there. He left Broadstairs the following day and was taken ill with the complaint on October 16th (the boys were taken ill in the school on October 13th).”
Given this, the virus-alone theory of polio has some heavy lifting to do in Broadstairs. It needs to explain how all these schools, with not much interaction between them, developed simultaneous polio epidemics; and why the disease was pretty much confined to those places, and institutions like the convalescent homes, but skipped the elementary schools – and the community at large. And why it lasted the same two weeks in all those locations.
I wish I knew more about the British education system – I’m always getting public and private and elementary and secondary mixed up -- but in my head I imagine a fairly evolved system of food delivery to schools and other institutions like convalescent homes, schools, restaurants, hotels ... Since the disease broke out around harvest time, let’s pick apples as a source and let's blame lead arsenate as the poison; it had been used since 1892 in Boston to fight gypsy and coddling moths on apple trees. (By 1926, lead arsenate had already been suggested as a polio trigger more than once, from Boston to Australia.)
An orchard or a wholesale food distributor could have delivered apples from the same tainted batch to all these institutions. I imagine a vintage vehicle pulling up to the schools driven by a man in a white cap and coat with "Broadstairs Produce" on the side of the truck. I can see the waiter sitting down to the meal that came with the job and biting into a bright red apple. But why this year in this place? Let us count the ways: a poorly mixed batch of pesticide; an overzealous applicator; a drought that failed to rinse the produce before harvest; sheer bad luck of some kind with a toxin without much margin for error. Then, of course, the poliovirus needed to be circulating. One of the first students affected had recently returned from Brittany, so it's a possibility he picked up the virus in France and spread it widely at the start of school. It's also possible, of course, that a food handler with the virus spread it that way, offering up both polio and the poison in one serving.
The fact that the Broadstairs cases hit “particularly boarding schools” is important, since boarding students would have taken all their meals there, as opposed to the private day school students who would have gone home in the evening. And the fact the outbreak didn’t involve elementary schools is interesting, too. Did these younger kids go home for lunch and therefore never eat the same bad apples as their older schoolmates who got sick?
The fact the students lived at the boarding schools created more risk from contagion, I know. But the totality of evidence includes the waiter at the hotel and the headmaster’s brother-in-law who had lunch at a school. What’s the link? Food. (Even the woman who was visiting for two weeks was likelier to stay in a hotel or eat out than the average resident.) The age tally for the outbreak: “from 1 to 5 years, 7; 5 to 10 years, 18; 10 to 15 years, 27; 15 to 20 years, 5; 20 to 25 years, 2; 25 to 30 years, 3.” This skews older than usual for 1926, but it fits with the ages of the kids (and adults) who ate most of their food in institutional settings. The four deaths in Broadstairs tend to confirm the picture: “A boy, age 10, at a private boarding school; a woman, age 28, a teacher at a girls boarding school; a boy, aged 8, a day scholar at a private day and boarding school; a boy, aged 5, who attended the infant department of an elementary school.”
As I described in earlier articles, adults usually don’t get poliomyelitis (remember Mrs. Franklin, 56, and her ice cream store in Brooklyn?). That makes them anomalies. Anomalies make good clues. The waiter, the headmaster's brother-in-law, the visitor, the mistress, the domestic staff point firmly in the same direction -- food. That’s as far as the information at hand allows us to speculate, but the model we developed from 1916 has shown some analytical value in this epidemic.
I find it quite amazing, actually, that someone in Broadstairs didn’t wake up in the middle of the night in October 1926 mumbling, “The waiter… the lunch guest, the boarding schools," and then sitting bolt upright with a shock of recognition, "It’s the food, dammit!” Of course in my view it was not just the food, it was the toxin in the food interacting to amplify the poliovirus in those with active infections. No one was even thinking about food, at least not in this way. The Polio Paradigm had already rolled all over it. Earlier I described the Johns Hopkins researcher who came very close to the truth, in my opinion, during the 1916 New York epidemic. The New York Times reported: “Dr. Hempel has a theory that candy, ice cream, fruit, and other uncooked foods that children eat, are primarily responsible for bringing the germ into the system. That theory will be fully tested when the physicians have completed their transmissions experiments.”
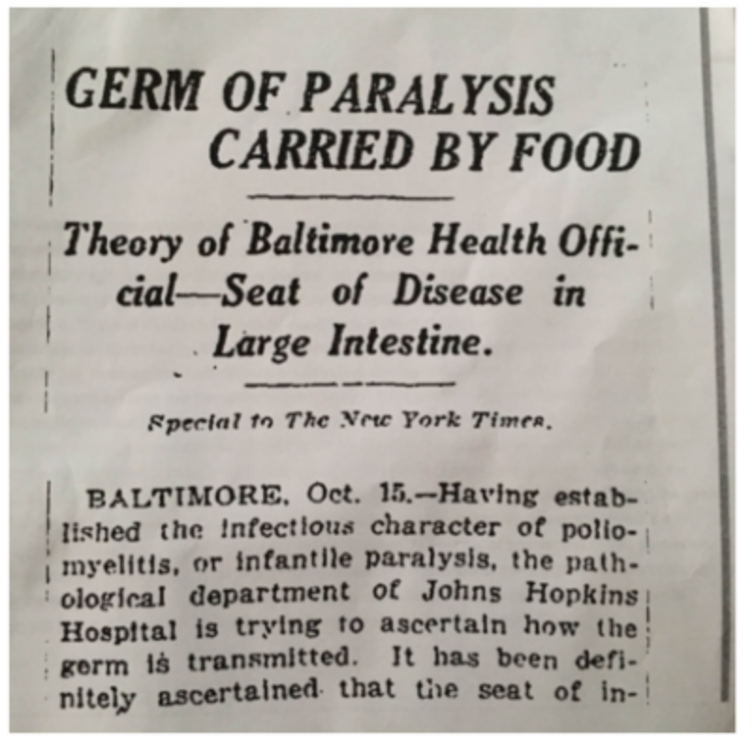
Dr. William H. Welch, head of the Hopkins medical faculty, fell on his sword in 24 hours under what must have been intense pressure from the New York City health establishment: “Denies Hopkins Rumors: Stories of Startling Discoveries in Paralysis Untrue, Dr. Welch Says." The Times quoted Welch saying that “the work which the Hopkins pathologists were doing in association with the physicians of the city health department on infantile paralysis had not developed anything that would change any views of the disease previously held.”
It’s so easy to suppress ideas. Have your dean dis you the day after your theory appears in the New York Times. Get your research canceled. (If any of this sounds familiar in regards to autism research or another field you're more familiar with, it should.) Then, ten years later in a different country, when a simultaneous outbreak at harvest time is confined to children who take their meals together at specific places, don't think about food, not even in you nightmares. Even when you toss in a waiter and a lunch visit by a brother-in-law!
As Russian anti-Putin performance artist Petr Pavlensky told the Daily Beast, "The methods are always the same. Officials reject, punish and humiliate people."
Today asking such questions still brings ridicule. Over at Respectful Insolence, the blogger Orac has been having fun with me. “I noted that Dan Olmsted is now up to part 12 (!) of his Age of Polio series, in which he tries to ‘prove’ that the polio vaccine didn’t save us. There’s no sign he’s done yet.” That’s right. I’m not done yet, and a little ridicule is not going to hurt my feelings. (And thanks for the link!) It's not true, however, that I disparage the polio vaccine. I believe it ended epidemics by knocking out the virus, though not the co-factor that amplified it in the first place. In a loose sense, medicine found the cure for poliomyelitis epidemics without fully understanding the cause or, you might say, it's real nature. And that failure has continued to wreak havoc.
15.
I’m gratified that so many of you are reading and commenting on the polio articles. To rustle up 61 comments this past weekend for the 14th installment is encouraging. If you haven’t followed along to date you are hereby absolved; this installment is not a bad place to catch up before we move into new territory. (And what does it have to do with autism? Read on.)
My aim is simple: to make an overwhelming case that arsenic was a co-factor in poliomyelitis outbreaks, and then to see what that tells us about not just polio but any number of things. The series to date presented evidence that the outbreak in New York City and the North Atlantic states in 1916 was triggered by arsenic pesticide from a Hawaiian sugar plantation that got into the food supply in the Northeast.
Those who take issue with the scenario I’ve presented – and I welcome the critiques because they make me stop and think – seem to have four different arguments:
- It’s just the poliovirus, not arsenic at all. The hygiene hypothesis explains why the virus got more virulent.
- It’s only the arsenic, the lead arsenate, the DDT and perhaps other 20th century pesticides that poisoned children. Not the poliovirus, at all. There was no viral aspect to "polio."
- There can be individual susceptibility to the virus, but it doesn't have to be arsenic. Maybe it's the physical effect of the sugar; or bad diets generally reducing kids’ immunity, or vaccines or lack of breastfeeding, as Cynthia Cornoyer suggested, or some other man-made intervention are responsible.
- (Courtesy of commenter VE who pointed to this alternative I overlooked: It wasn't polio virus and arsenic. It was Coxsackie virus and arsenic. Or some other virus/bacteria/munchkin and arsenic. What evidence is there to prove that polio virus was there in NYC 1916, causing all these paralysis and death cases? Detroit 1958 epidemic had taught us that when tested, there are several viruses to "blame" for the illness that is called "polio". So, I'm really curious: what evidence science can offer to establish it was polio virus in 1916?
The first idea, that the poliovirus causes poliomyelitis epidemics, period, is probably accepted by 99-percent-plus of experts and lay people. It is well expressed by our commenter Eindeker: “But you build a whole hypothesis on some speculative co-factor whereas the commonly accepted explanation for the polio outbreaks in cities in the early 20th C is bizarrely improved hygiene and sanitation … There is no need to invoke some speculative co-factor (arsenic et al) in changes in polio epidemiology during the 20th Century, unless you classify increasing hygiene and reduced exposure at a young age, as a co-factor.”
Eindeker’s critique makes me think of Occam’s razor, one of my own favorite principles – that the simplest explanation is usually correct. In this instance Eindeker is saying, as I read it, that I'm in violation of Occam's rule, because there is “no need” to cook up a co-factor to go with the virus. It's necessary and sufficient without it.
Except it's not. In my epigraph to the series I invoke Einstein’s view that “things should be made as simple as possible, but not simpler.” As the AOA reader and environmental toxicologist who's been helping it out put this theory: "People exposed to arsenic and the polio virus simultaneously will develop a worse case of polio than if they had not been exposed to the arsenic.” She elaborated: "A co-exposure is a situation in which a person is exposed to two different agents which interact and cause a response that is different than if the person had only been exposed to one of the agents. This seems to be playing out with Zika virus right now: the rate of microcephaly in Columbian infants exposed to Zika in utero is at this point lower than the rate for Brazilian infants, which implies that there is a second factor involved in the Brazilian cases.
"Contemporaneous observers were surprised to see the polio virus turn deadly, because it had previously been thought to be relatively benign. What you are pointing out is that polio epidemics became deadly right around the same time as the use of heavy metal pesticides on agricultural crops took hold. The use of lead arsenate in American orchards is known, but your research has dug up the fact that arsenic was used in the sugar cane fields. Sugar is a somewhat unique crop because it ends up in concentrated form, so impurities can get concentrated too. In NYC in 1916, arsenic wasn’t really 'circulating'; exposure would have been irregular. However, the virus may have been circulating. The most obvious mechanism for the arsenic is that, by causing GI problems, it facilitated the virus’ crossing of the intestinal barrier. Remember that it takes time for an unexposed person to mount an effective immune challenge to any infectious agent. If the virus crossed the intestinal barrier at a faster rate because of pre-existing damage done by arsenic, then the unexposed person’s immune system might be overwhelmed, and the damage would already be done before the immune system had a chance to get rolling."
In the same way I believe, based on reporting and research by many people (including myself), that autism is an environmentally triggered illness, involving metals like mercury and aluminum and live viruses like the MMR and chickenpox. They amplify and potentiate each other. They make it far more likely that an infant vaccinated with a grossly excessive stew of viruses and toxins, especially metals, is primed for a fall. Even the exposure path from the gut to the nervous system may be relevant to autism.
The second critique of the arsenic-virus theory is the toxin-only critique -- there’s no such thing as a poliovirus, or if there is it doesn’t trigger epidemics of paralytic illness; therefore, the “vaccine” didn’t really end those epidemics. Under this theory, It was banning DDT that caused the epidemics to diminish. Cases were camouflaged as "flaccid paralysis."
The third objection is that there could have been a co-factor, but it didn't have to be arsenic. That is true. I went looking for arsenic in association with the 1916 outbreak and think I found a strong connection. Still, this entire exercise could be a prime example of confirmation bias, causing me to decide a small sugar plantation in Hawaii somehow triggered the great Northeast epidemic of 1916 by using arsenic to kill weeds. Say what? (The fourth objection -- it was a virus, but not the poliovirus -- is also worth more scrutiny but is not central to whether my arsenic hypothesis stands or falls.)
But it's also true one needs confidence in one's theories until and unless they lose their explanatory power, as Karl Popper wrote. "Propose theories which can be criticized. Think about possible decisive falsifying experiments—crucial experiments. But do not give up your theories too easily—not, at any rate, before you have critically examined your criticism."
So please keep offering your critiques, which I'll keep critically examining as we head further into a world where things are not what they seemed.
###
A note for those of you expecting the latest installment in the polio series – I’m taking a break to complete another project but will return with a vengeance in a while. I’ve pretty much completed the arc of the 1916 New York City and North Atlantic epidemic, proposing that sugar tainted with arsenic pesticide triggered the outbreak in those with an active poliovirus infection. Next we’ll look at other outbreaks to test and refine our hypothesis, and ultimately examine why polio is the autism of childhood illnesses, and autism is the polio of childhood disorders – both triggered by an environmental factor that orthodox medicine is either slow to recognize or suppresses altogether. I guess you could call it an after-action report; it's all about "hindsight "that should have been just as clear at the time if the experts weren't blinded by their own theories at the cost of ignoring the people right in front of them.
--
For the rest of this article please go to source link below.