Spotlight on Implanon and Mirena long-acting reversible contraceptives, as women report severe side-effects
 Long-acting reversible contraceptives have been growing in popularity in recent years.
Long-acting reversible contraceptives have been growing in popularity in recent years.
There are growing fears about serious side-effects from two popular contraceptive devices, with claims concerns are being glossed over by pharmaceutical companies.
Key points:
- The products are known as long-acting reversible contraceptives and have grown in popularity
- The ABC has found pharmaceutical companies have been waging massive marketing campaigns to promote the devices
- Some women claim the impact on their mental health meant they have had to take anti-anxiety medication for the first time in their lives
An ABC investigation has found women around the country are reporting serious concerns about the Implanon hormonal arm implant and Mirena intra-uterine devices.
Their concerns include chronic pain, pelvic inflammatory disease, serious scarring and depression.
Of more than 945,000 Implanon devices inserted in Australia over the past decade the Therapeutic Goods Administration has received more than 1,000 reports from treating doctors and specialists of side-effects and other problems.
These include more than 500 unintended pregnancies, more than 50 vaginal haemorrhages and 27 ectopic pregnancies.
Of more than 967,000 Mirena devices implanted in the past decade the Therapeutic Goods Administration has received more than 850 reports of adverse effects.
These include 70 pregnancies and more than 100 uterus perforations.
Affected women have told the ABC when they have asked to have the devices removed some doctors have resisted because they believe patients adapt to the hormones and most side-effects subside.
 This woman experienced severe scarring and required stitches after the removal of an Implanon.
This woman experienced severe scarring and required stitches after the removal of an Implanon.
The products are known as long-acting reversible contraceptives, or LARCs, and have been growing in popularity in recent years.
Unlike traditional contraceptive pills, these devices are often still under patent and do not have any competition.
The ABC has found pharmaceutical companies have been waging massive marketing campaigns to promote the devices.
It includes paying key opinion leaders for consultancy work, sponsoring educational events for advocacy groups, general practitioners and specialists and getting favourable press through health forums.
As recently as September 2017, the major industry group representing hospitals, the Australian Healthcare and Hospitals Association, issued a public statement they called a "Consensus Statement" on the use of LARCs for World Contraceptive Day.
It stated a number of goals including reducing unplanned pregnancies by, "increased access to long-acting reversible contraceptive methods".
The statement was backed the College of Midwives, Nurse Practitioners, the Royal Australian New Zealand College of Obstetricians and Gynaecologists, Family Planning NSW, Health Consumers Council and even Marie Stopes Australia.
At the end of the statement the association disclosed it was, "supported by the funding from Merck Sharp & Dohme (MSD)" and developed during a health forum where MSD and Bayer Pharmaceuticals were participants.
MSD makes one of the major LARCs on the market — Implanon. Bayer makes the other major device, Mirena.
The statement came despite most experts conceding contraceptive choice was highly individual.
When the ABC questioned the Australian Healthcare and Hospitals Association, it agreed it was a personal choice but added the statement was about reflecting "systemic factors" that prevented women learning about the devices, not influencing doctors.
'All up it was seven months straight pretty much that I bled'
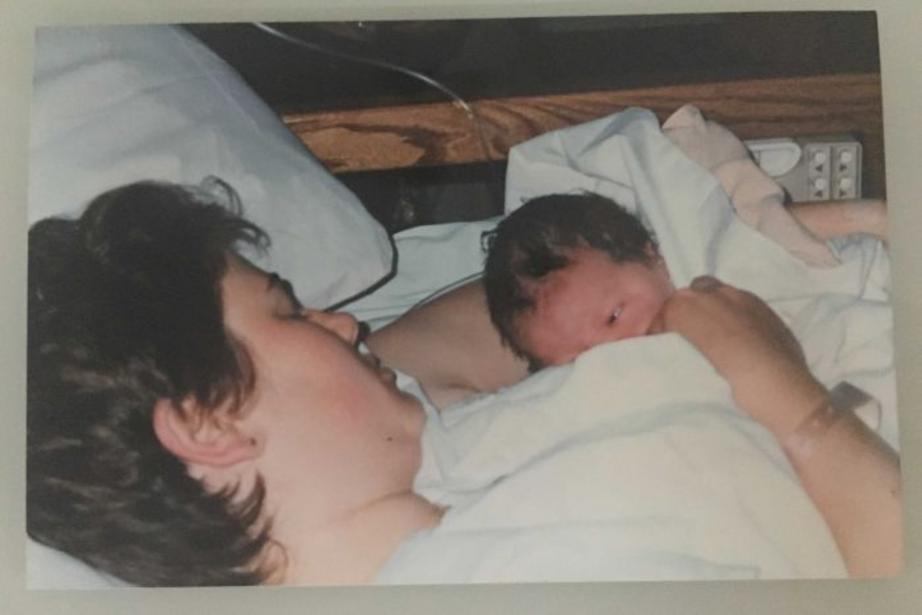
Implanon was not the answer for mother-of-four Suzie Short.
She had just had her first baby when her GP suggested she have the implant, which lasts three years, in her arm.
 Mother of four Suzie Short tried the Implanon implant in between children and says she still experiences serious side effects.
Mother of four Suzie Short tried the Implanon implant in between children and says she still experiences serious side effects.
"Probably about two months after, I started bleeding non-stop," she said.
"All up it was seven months straight pretty much that I bled."
Ms Short was so lethargic she could not care for her infant daughter and said she believed her body reacted to the progesterone in the implant that prevents ovulation.
Many years later she is still struggling from side-effects and attributes them to the device.
"I've now got chronic pelvic pain due to adhesions, all of my abdominal organs are fusing to my abdominal wall, I've had pelvic inflammatory disease, I've had an abscess in my right fallopian tube," she said.
Ms Short is also on anti-depressants and resents the impact the medication has had on her ability to parent.
"I can't just go and play with my kids," she said.
She is a member of a Facebook page of more than 700 women who say they've suffered serious side-effects from Implanon, including serious scarring after removals.
In a statement a spokeswoman for Implanon's maker Merck, Sharpe and Dohme told the ABC: "The approved Product Information for Implanon provides guidance on appropriate use in suitable patients."
"Patients should speak to their healthcare professional about their contraceptive options," she said.
'Day one, severe cramping, the bleeding was bad'
Implanon is not the only device under the spotlight.
More than 700 Australian women are in support group for fallout from a hormone-release intra-uterine device called a Mirena, which lasts five years.
 Brisbane mother Jane Morgan-Harry says she has had serious side effects from a Mirena intra-uterine device.
Brisbane mother Jane Morgan-Harry says she has had serious side effects from a Mirena intra-uterine device.
Mother-of-three Jane Morgan-Harry was lying in hospital after a miscarriage when her doctor suggested she try a Mirena.
Ms Morgan-Harry said she had asked to have her tubes tied but her doctor had just returned from a medical conference on the device.
"My state of mind was I didn't want to have to go through what I'd just gone through," she said.
After the procedure Ms Morgan-Harry knew she had made a mistake.
"So, day one, severe cramping, the bleeding was bad," she said.
"I had headaches, sweats, the shakes, nausea continuously pretty much 24 hours a day.
"Honestly sometimes the hormones are like I'm going through menopause."
She claims the impact on her mental health meant she had to take anti-anxiety medication for the first time in her life.
 Ms Morgan-Harry said she was convinced by a doctor who had just returned from a medical conference.
Ms Morgan-Harry said she was convinced by a doctor who had just returned from a medical conference.
Ms Morgan-Harry spent months trying to get a doctor to listen to her and agree to remove it.
"The response was pretty much I was making it up, that it can't be from the Mirena," she said.
"I'm pretty angry because I knew what was happening."
Her period now lasts for two weeks each month but she will have to wait more than a year to have the device removed in a public hospital.
 The Mirena Device inside Brisbane mother Jane Morgan-Harry that she wants removed after experiencing years of severe side effects.
The Mirena Device inside Brisbane mother Jane Morgan-Harry that she wants removed after experiencing years of severe side effects.
In a statement Bayer, the makers of Mirena, said millions of women worldwide had used the device, "But like any prescription product, Mirena has risks and benefits".
"We investigate reports on side-effects thoroughly and collaborate closely with the Therapeutic Goods Administration concerning the use, benefits and risks of all products," a spokeswoman said.
So why the push the for LARCS?
For a long time the main two players in the market for traditional contraceptive pills have been pharmaceutical giants Bayer and Pfizer.
But in recent years they've had extra competition from the generic market.
So now the main players are increasingly focusing their attention on Long-Acting Reversible Contraceptives or LARCs.
Bayer makes Mirena, MSD make Implanon and Pfizer make long-acting contraceptive injections, commonly known as Depo-Provera.
All three companies have been spending up big as they jockey for market share.
Symposiums, seminars and societies
An ABC analysis of Pharmaceutical Company reports show all three companies have been working to get their brands in front of those that prescribe these contraceptives.
Reports submitted to industry group Medicines Australia show the companies each spent large sums to sponsor events attended by medical professionals.
In 2015, MSD spent more than $150,000 on sexual health educational programs for doctors.
The next year its spending included $30,000 sponsoring a sexual health GP mentoring program at the Pullman Hotel in Sydney.
In 2016, Bayer spent $12,000 on a Trade Display at the RANZCOG Annual scientific Meeting in Crown Casino's Perth Hotel.
It also spent $4,077 for 60 Marie Stope International doctors to attend dinner meetings including one at the Bottega Restaurant in Melbourne.
Back in 2015, it alone splashed out more than $220,000 on a range of "contraception counselling" and similar seminars and society meetings that reached more than 7,500 doctors and nurses.
Pfizer spent more than $20,000 on trade displays at Women's Health Conferences in Brisbane and Adelaide.
The companies maintain they have no input into the meetings and need to run education programs to teach doctors about their products.
 Dr Barbara Mintzes says evidence shows promotional events have had some influence on prescribing habits.
Dr Barbara Mintzes says evidence shows promotional events have had some influence on prescribing habits.
Dr Barbara Mintzes, from the Faculty of Pharmacy at the University of Sydney said evidence showed these promotions did influence prescribing habits.
"The aim of those payments would be to increase the rate of use of those long-acting contraceptives," she said.
"When it comes to contraception it's a bit different from other medical treatments … not everyone needs a same method," she said.
Family Planning NSW says while they had received sponsorships it hadn't influenced its independent advice.
It said in a statement: "Our evidence-based advice is developed through thorough review of the academic literature."
Marie Stopes Australia's medical director, Dr Philip Goldstone, told the ABC the dinners its doctors attended discussed a number of issues, not just long-acting contraceptives, and the service always put patients first.
"The method of contraception is based on the patient's individual circumstances," he said.
Bayer said it complied with relevant codes of conduct when it came to sponsorships.
"We believe that the medical community benefits greatly from the support provided by industry," a spokeswoman said.
MSD said it followed reporting requirements when it came to the funding of educational events.
"This education and training assists healthcare professionals to have informed discussions with their patients," a spokeswoman said.
College defends promotion of new contraceptives
 Another woman's arm was left with bruising which was visible for several days after removal.
Another woman's arm was left with bruising which was visible for several days after removal.
The Royal Australian New Zealand College of Obstetricians and Gynaecologists said the side-effect reports by women were "not typical".
Dr Amber Moore from the college said women with Implanon should only get a tiny scar similar to a vaccination scar.
"They provide a great deal of a certainty for women in terms of safety against pregnancy, and they're incredibly cost-effective," she said.
"After the first few months … most women will in fact end up never going through another packet of pads or tampons.
"All the studies internationally and here have indicated that women like them because they go back in, they have another one."
She said doctors should be following patient requests to remove devices.
Dr Moore defended the consensus statement.
"It's based on high levels of science," she said.
"The fact that there was some financial support from the manufacturer has not influenced the information."

