Magnesium and K2 optimize your vitamin D supplementation
Story at-a-glance
- If you take supplemental vitamin D3, you also need to be mindful of taking extra vitamin K2 and magnesium
- It’s important to increase your vitamin K2 intake when taking high-dose supplemental vitamin D to avoid complications associated with excessive arterial calcification
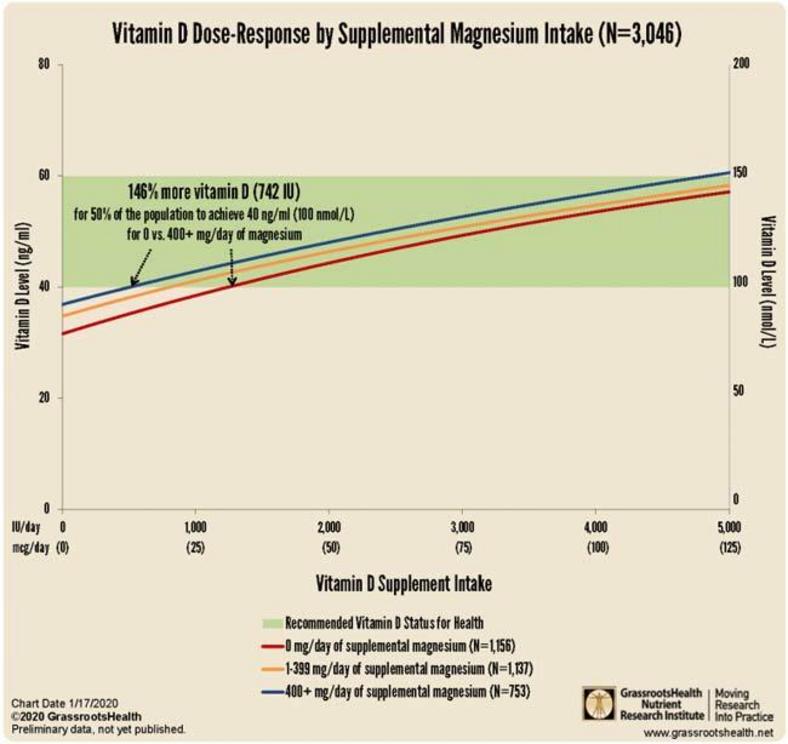
- You need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day
- Vitamin D improves magnesium absorption, but taking large doses of vitamin D can deplete magnesium, as magnesium is required in the conversion of vitamin D into its active form
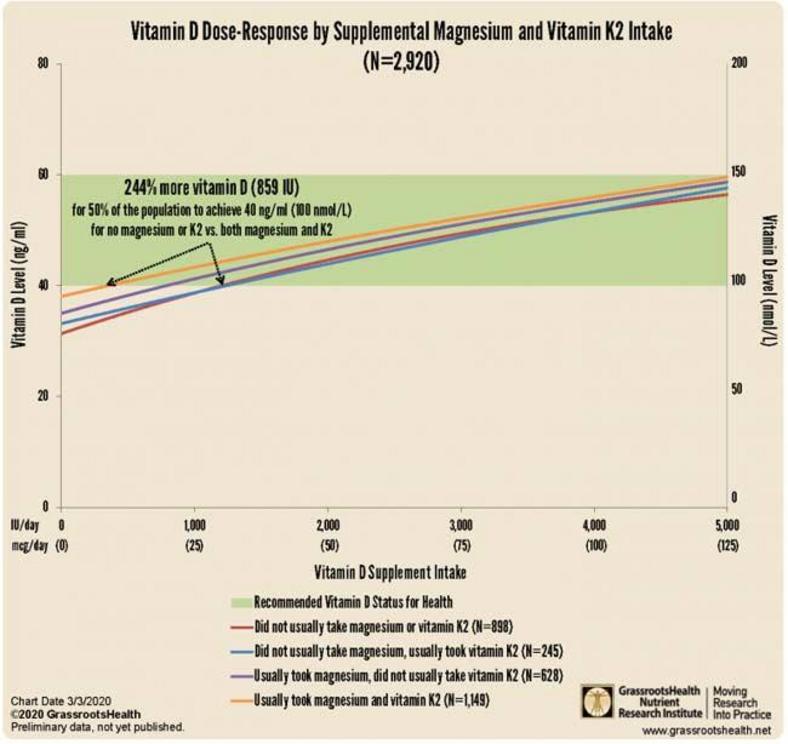
- Combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually. You need 244% more oral vitamin D if you’re not concomitantly taking magnesium and vitamin K2
Optimizing your vitamin D level is ideally done through sensible sun exposure. However, many simply are unable to obtain sufficient levels from the sun alone and need supplemental vitamin D. In this case, nutritional synergies become an important factor.
According to research by GrassrootsHealth,1 “combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually,” and “those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither.”
You Need 2.5 Times More D if Not Taking Magnesium and K2
GrassrootsHealth is a nonprofit, independent public health research institute that has been conducting large-scale population-based nutrient research since 2007.2 While a significant focus is on vitamin D, the organization has also branched into other nutrients.
Its D*action project includes a global cohort of over 10,000 self-subscribed individuals who, anonymously, provide information about their supplement use and overall health status.
GrassrootsHealth research shows blood levels in the range of 40 nanograms per milliliter to 60 ng/ml (100 nanomoles per liter to 150 nmol/L) are safe, effective and will lower overall disease incidence and health care costs.3
That said, other nutrients have been shown to work synergistically with vitamin D, and being deficient in them can significantly influence your vitamin D status as well. Importantly, data from nearly 3,000 individuals reveal you need 244% more oral vitamin D if you’re not also taking magnesium and vitamin K2. As reported by GrassrootsHealth:4
“… 244% more supplemental vitamin D was needed for 50% of the population to achieve 40 ng/ml (100 nmol/L) for those not taking supplemental magnesium or vitamin K2 compared to those who usually took both supplemental magnesium and vitamin K2.”
What this means in practical terms is that if you take all three supplements in combination, you need far less oral vitamin D in order to achieve a healthy vitamin D level.
How Magnesium Affects Vitamin D
I’ve previously written about the importance of taking vitamin K2 when you’re taking high-dose supplemental vitamin D to avoid complications associated with excessive calcification in your arteries. In fact, relative vitamin K2 deficiency is typically what produces symptoms of “vitamin D toxicity.”
That said, magnesium is also a crucial part of the equation, as it is a component necessary for the activation of vitamin D. Without sufficient amounts of it, your body cannot properly utilize the vitamin D you’re taking.5,6,7,8
This actually helps explain why many need rather high doses of vitamin D to optimize their levels — it could be that they simply have insufficient amounts of magnesium in their system to activate the vitamin D. As noted by Mohammed Razzaque, professor of pathology at Lake Erie College of Osteopathic Medicine in Pennsylvania:9
"People are taking vitamin D supplements but don't realize how it gets metabolized. Without magnesium, vitamin D is not really useful. By consuming an optimal amount of magnesium, one may be able to lower the risks of vitamin D deficiency, and reduce the dependency on vitamin D supplements.”
According to a scientific review10,11 published in 2018, as many as 50% of Americans taking vitamin D supplements may not get significant benefit as the vitamin D simply gets stored in its inactive form, and the reason for this is because they have insufficient magnesium levels.
Research published in 2013 also highlighted this issue, concluding that higher magnesium intake helps reduce your risk of vitamin D deficiency by activating more of it. As noted by the authors:12
“High intake of total, dietary or supplemental magnesium was independently associated with significantly reduced risks of vitamin D deficiency and insufficiency respectively.
Intake of magnesium significantly interacted with intake of vitamin D in relation to risk of both vitamin D deficiency and insufficiency … Our preliminary findings indicate it is possible that magnesium intake alone or its interaction with vitamin D intake may contribute to vitamin D status.”
Similarly, GrassrootsHealth has found13 you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
The interplay between magnesium and vitamin D isn’t a one-way street, though. It goes both ways. Interestingly, while vitamin D improves magnesium absorption,14 taking large doses of vitamin D can also deplete magnesium.15 Again, the reason for that is because magnesium is required in the conversion of vitamin D into its active form.
Vitamins D, B12 and Magnesium May Affect COVID-19 Outcomes
While vitamin D and magnesium are important for overall health year-round, they may be of particular importance right now, as we’re still dealing with the COVID-19 pandemic in many areas of the world, and a second wave is expected in the fall.
According to preliminary research,16,17 that is still undergoing peer review, older COVID-19 patients given a combination of vitamin D, magnesium and vitamin B12 fared significantly better than those who did not receive the supplements:
“Between 15 January and 15 April 2020, 43 consecutive COVID-19 patients aged ≥50 were identified. 17 patients received DMB [vitamin D, magnesium and B12] and 26 patients did not. Baseline demographic characteristics between the two groups were similar.
Significantly fewer DMB patients than controls required initiation of oxygen therapy subsequently throughout their hospitalization (17.6% vs 61.5%). DMB exposure was associated with odds ratios of 0.13 … and 0.15 … for oxygen therapy need and/or intensive care support on univariate and multivariate analyses respectively.
Conclusions: DMB combination in older COVID-19 patients was associated with a significant reduction in proportion of patients with clinical deterioration requiring oxygen support and/or intensive care support. This study supports further larger randomized control trials to ascertain the full benefit of DMB in ameliorating COVID-19 severity.”
Signs of Vitamin D Deficiency
The idea that vitamin D might play a role in COVID-19 severity makes sense considering its importance in infections, including viral infections, in general. Vitamin D helps regulate your immune function, and deficiency is associated with more frequent infections and inflammation-related illnesses of all types. Other common signs and symptoms of vitamin D deficiency include:18
- Muscle weakness and fatigue
- Bone and joint pain, as well as fractures
- Depression
- Impaired cognition and headaches
- Slow wound healing
To improve your immune function and lower your risk of viral infections, you’ll want to raise your vitamin D to a level between 60 ng/mL and 80 ng/mL by fall. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L. Optimizing your vitamin D is particularly important if you are older or have darker skin.
Long-term deficiency can also contribute to more chronic health problems, including rickets, cardiovascular disease and autoimmune disease.19 Risk factors for vitamin D deficiency include:
- Rarely spending time outdoors and/or always wearing sunscreen
- Having darker skin
- Being over the age of 50
- Obesity
- Having gastrointestinal problems
Optimize Your Vitamin D Before Fall
Aside from age and comorbidities such as diabetes, obesity and heart disease, vitamin D deficiency has also been identified as an underlying factor that significantly impacts COVID-19 severity and mortality. I discuss this in “Vitamin D Is Directly Correlated to COVID-19 Outcome.”
The following graph is from a May 18, 2020, letter20 to the Federal Chancellor of Germany, Angela Merkel, from retired biochemist Bernd Glauner and Lorenz Borsche, in which they highlight studies21 showing a clear correlation between COVID-19 mortality and vitamin D levels.
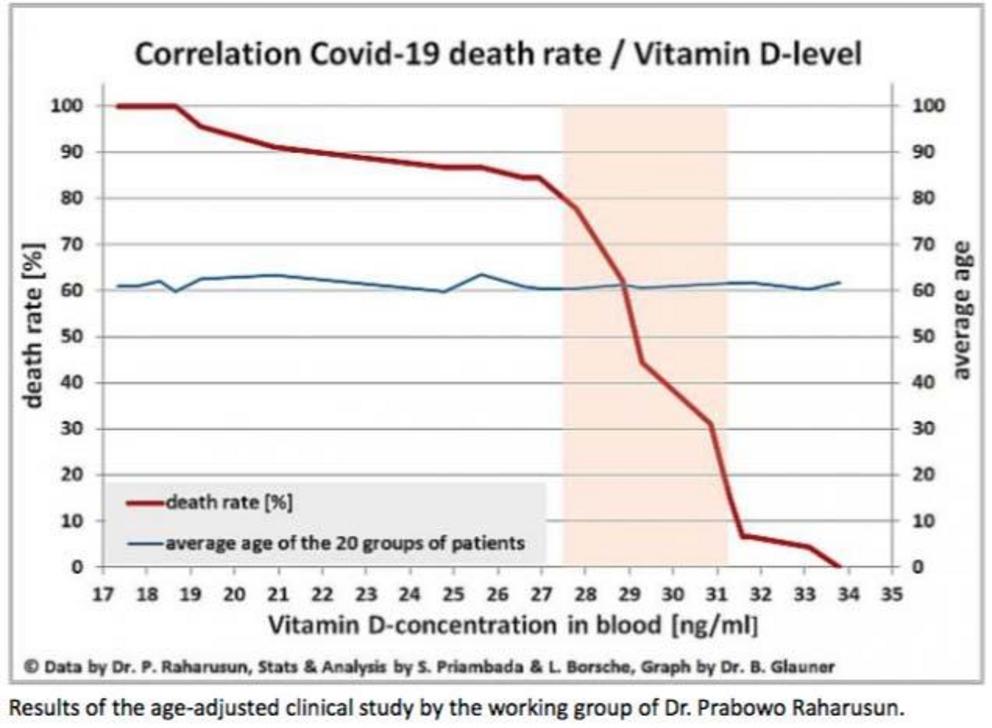
It’s important to note that experts are already warning SARS-CoV-2 may reemerge in the fall when temperatures and humidity levels drop, thereby increasing the virus’ transmissibility.
To improve your immune function and lower your risk of viral infections, you’ll want to raise your vitamin D to a level between 60 ng/mL and 80 ng/mL by fall. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L. Optimizing your vitamin D is particularly important if you are older or have darker skin.
One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit, either alone or in combination with the omega-3 test. This is done in the convenience of your home.
To make sure your vitamin D level and immune system function are optimized, follow these three steps:
1. First, measure your vitamin D level — Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. The easiest way to raise your level is by getting regular, safe sun exposure, but if you’re very dark-skinned, you may need to spend about 1.5 hours a day in the sun to have any noticeable effect.
Those with very light skin may need only 15 minutes a day, which is far easier to achieve. Still, they too will typically struggle to maintain ideal levels during the winter. So, depending on your situation, you may need to use an oral vitamin D3 supplement. The next question then becomes, how much do you need?
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, consider using the DMinder app.22
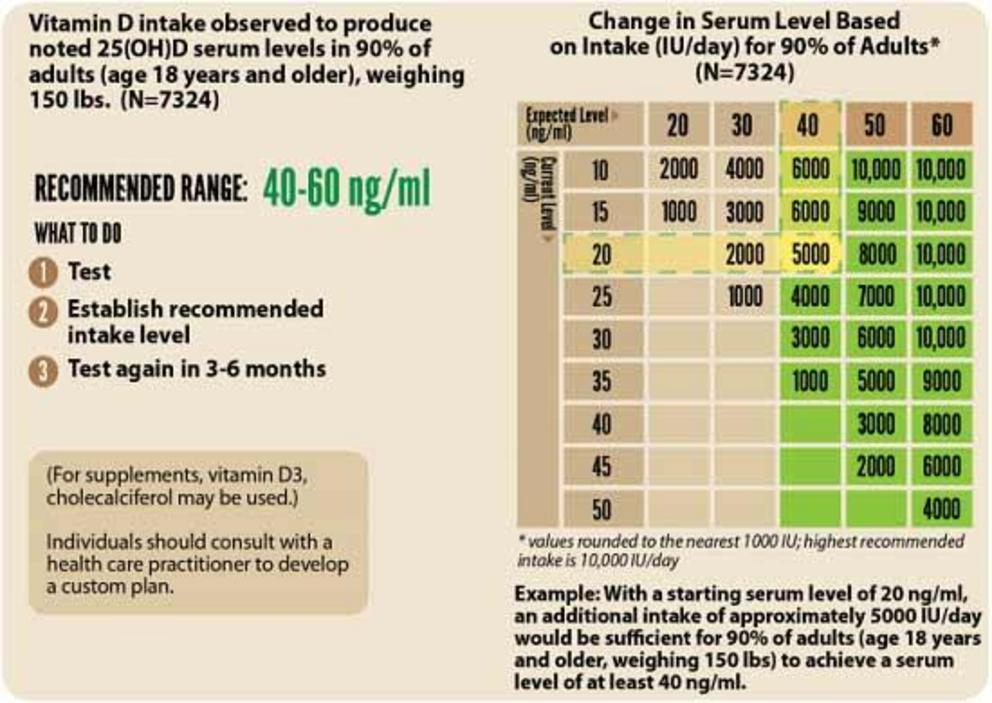
3. Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
Not only will optimizing your vitamin D be an important strategy for you and your family, but it would be really helpful to start thinking about your community as well.
If you can, speak to pastors in churches with large congregations of people of color and help them start a program getting their congregation on vitamin D, and if you have a family member or know anyone who is in an assisted living facility, meet with the director of the program and encourage them to get everyone tested or at least start them on vitamin D.
I am currently in the process of writing a comprehensive resource book to help you in this effort. We really need an army of people to make a difference and build up the immune resiliency of the population before the next wave hits in the fall. This will work FAR better than any unsafe and untested vaccine that will most likely never be ready by the fall anyway.
For full references please use source link below.

