Curbing Candida: the cells that keep fungal infections at bay
Without cells that spur on the specialized antifungal units, the fight against a common infection is a lost cause
Curbing Candida: The Cells That Keep Fungal Infections at Bay
- Jakub Abramson
- Immunology and Regenerative Biology
- Yeast cells
- Candida
- Infectious diseases
- Immune cells
- Autoimmune
Of all the fungi that live in the human body, the most infamous is probably the yeast Candida. This distant cousin of baker’s yeast is notorious for causing various types of thrush that can be a major nuisance, but it can also lead to an invasive infection that may, on occasion, prove fatal. In a study published today in Nature Immunology, a Weizmann Institute of Science research team headed by Prof. Jakub Abramson uncovered a previously unknown defense mechanism employed by the immune system in fighting Candida infections.
(l-r) Prof. Jakub Abramson, Osher Ben-Nun, Dr. Yael Goldfarb, Tal Givony and Amit Binyamin
Candida is present at low levels in the bodies of most healthy people, forming part of the microbiome – a diverse spectrum of microbes that reside peacefully in our gut and on our skin. Under normal circumstances, Candida is held in check by the immune system, but it can occasionally grow excessively, invading the lining of the mouth, the vagina, the skin or other parts of the body. In severe cases, it can spread to the bloodstream and from there to the kidneys. Such life-threating infections may occur when a person’s immune system has been weakened, for example, by AIDS or by immunosuppressive drugs such as cancer chemotherapy or steroids. Antibiotics, which wipe out many of the beneficial bacteria within our microbiome, can also unleash local or invasive Candida eruptions by providing this yeast with an unfair advantage vis-à-vis other microorganisms. That’s why, for instance, women sometimes develop a vaginal yeast infection after taking antibiotics.
Until now, the immune cells that got most of the credit for defending the body against Candida were the small, round lymphocytes of the T cell type, called TH17. These cells were also the ones to take the blame when this defense failed.
In the new study, postdoctoral fellow Dr. Jan Dobeš, working together with colleagues in Abramson’s lab in Weizmann’s Immunology and Regenerative Biology Department, discovered that a powerful commando unit of TH17 cells capable of fighting Candida cannot be generated without crucial early support from an entirely different contingent: a subset of rare lymphoid cells known as type-3 innate lymphoid cells, or ILC3, that express a gene called the autoimmune regulator, or Aire
The two groups of cells belong to the two different arms of the immune system, which, like foot patrols and specialized units, join forces against a common enemy. The Aire-ILC3s – part of the more ancient, innate arm – spring into action almost immediately upon encountering a threat – in this case, a Candida infection. The TH17s belong to the immune system’s more recent, adaptive arm, which takes several days or even weeks to respond, but which launches a much more targeted and potent attack than the innate one.

Dr. Jan Dobeš
The scientists found that as soon as Candida starts infecting tissues, the Aire-ILC3s engulf the yeast whole, chop them up and display some of the yeast pieces on their surfaces. That’s how these bits are presented to the TH17s, a few of which are generally on call in the lymph nodes, ready for an infection alert. This kind of presentation instructs the specialized T cells to start dividing rapidly, soaring in number from a few lone commandos to several hundred or even thousands of Candida-specific fighters, capable of destroying the yeast at the sites of infection.
“We have identified a previously unrecognized immune system weapon that is indispensable for orchestrating an effective response against the fungal infection,” Abramson says.
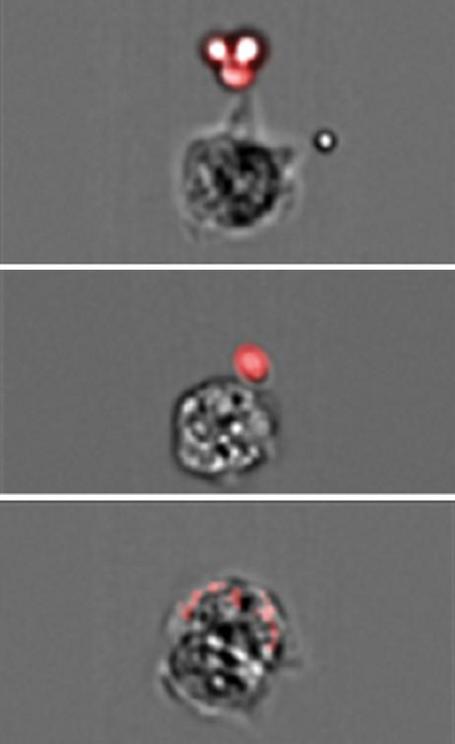
An Aire-ILC3 cell (gray) captures and swallows a Candida cell (red)
Abramson became intrigued by Candida because it commonly leads to severe, chronic infections in people with a rare autoimmune syndrome caused by defects in the Aire gene. Abramson’s lab had conducted extensive studies of this gene, helping to clarify its role in preventing autoimmune disorders. That research, as well as studies by other scientists, had shown that Aire-expressing cells in the thymus instruct developing T cells to refrain from attacking the body’s own tissues. When Aire is defective, T cells fail to receive proper instructions, consequently causing widespread autoimmunity that wreaks havoc in multiple body organs. But one puzzle remained: Why would Aire-deficient patients suffering from a devastating autoimmune syndrome also develop chronic Candida infections?
While trying to complete the Aire puzzle, Dobeš and colleagues found that outside the thymus, Aire is also expressed in a small subset of ILC3s in the lymph nodes. The researchers then genetically engineered two groups of mice: One lacked Aire in the thymus, and the other group lacked it in the ILC3s in the lymph nodes. The first group developed autoimmunity but was able to successfully fight off Candida. In contrast, those in the second group, the ones lacking Aire in ILC3s, did not suffer from autoimmunity, but were unable to generate numerous Candida-specific TH17s. Consequently, they failed to effectively eliminate Candida infections. In other words, without Aire-expressing ILC3s, the specialized T cells needed for fighting Candida were not produced in sufficient numbers.
“We found an entirely new role for Aire, one that it plays in the lymph nodes – turning on a mechanism that increases the numbers of Candida-fighting T cells,” Dobeš explains.
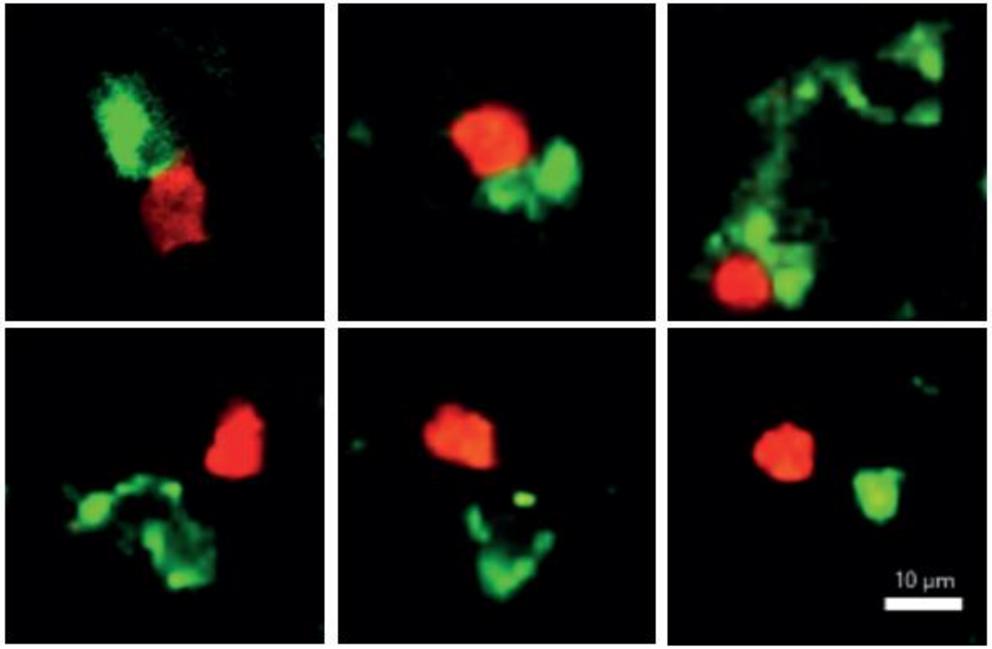
An Aire-ILC3 cell (green) "kisses" a Candida-fighting TH17 cell (red), telling it to start dividing (top row), but it ignores other T cells that do not specialize in fighting Candida (bottom row)
These findings open up new directions of research that in the future may help develop new treatments for severe Candida, and possibly for other fungal infections. The newly discovered mechanism might, for example, help produce large numbers of Candida-fighting T cells to be used in cell therapy. And if scientists one day identify the signals by which Aire-ILC3s boost T cell proliferation, these signals themselves might provide the basis for new therapies.
Study participants also included Osher Ben-Nun, Amit Binyamin, Dr. Yael Goldfarb, Dr. Noam Kadouri, Yael Gruper, Tal Givony and Itay Zalayat of Weizmann‘s Immunology and Regenerative Biology Department; Dr. Liat Stoler-Barak and Prof. Ziv Shulman of the Systems Immunology Department; Katarína Kováčová, Helena Böhmová and Evgeny Valter of Charles University, Prague; Bergithe E. Oftedal and Prof. Eystein S. Husebye of the University of Bergen, Norway; and Dr. Dominik Filipp of the Institute of Molecular Genetics of the Czech Academy of Sciences, Prague.
Science Numbers
Candida causes about 25% of hospital deaths and is the major cause of mortality in people with AIDS. It is responsible for more than 90% of vaginal infections and for nearly 100% of diaper rashes.
Prof. Jakub Abramson's research is supported by the Dr. Dvora and Haim Teitelbaum Endowment Fund; the Sy Syms Foundation; and the David E. Stone and Sheri Hirschfield Stone 75th Anniversary Fund. Prof. Abramson is the incumbent of the Eugene and Marcia Applebaum Professorial Chair.