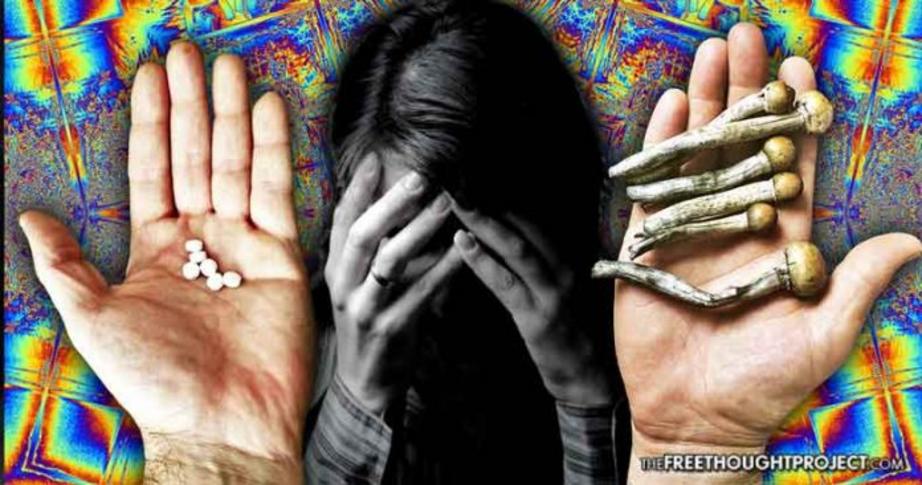
New study reveals mushrooms cure depression by doing the exact opposite of anti-depressants
A recent study shows that psilocybin-assisted therapy mitigates depression by increasing emotional connection—the exact opposite of anti-depressants.
A revolutionary new study is once again revealing a natural approach to be far superior to big pharma solutions—this time involving psilocybin, the active compound in magic mushrooms.
The study, published in the scientific journal Neuropharmacology, found that clinically depressed people had increased neural responses to fearful faces one day after a psilocybin-assisted therapy session, which positively predicted positive clinical outcomes.
“Psilocybin-assisted therapy might mitigate depression by increasing emotional connection,” neuroscientist and study author Leor Roseman, a Ph.D. student at Imperial College London, explained to PsyPost.
This is almost the exact opposite of how standard anti-depressants operate, as SSRI’s typically work by creating an “emotional blunting.”
“[T]his is unlike SSRI antidepressants which are criticized for creating in many people a general emotional blunting,” noted Roseman.
“I believe that psychedelics hold a potential to cure deep psychological wounds, and I believe that by investigating their neuropsychopharmacological mechanism, we can learn to understand this potential,” explained Roseman.
The study examined 20 individuals diagnosed with moderate-to-severe treatment-resistant depression, in an effort to investigate how psilocybin would affect brain activity and chronic depressive symptoms.
According to a report by Science Alert:
Psilocybin, the active compound in magic mushrooms, has long been known to deliver therapeutic effects to people with depression, and researchers think this is because the drug helps to revive emotional responsiveness in the brain.
What’s so remarkable is this kind of mechanism is actually the opposite effect of a major class of antidepressants used to treat the condition, called selective serotonin reuptake inhibitors (SSRIs).
Some of the same researchers, in a previous study, revealed that psilocybin seems to ‘reset’ brain circuits in depressed people. In that study, patients reported the benefits of psilocybin lasted up to five weeks after ending the treatment.
In the most recent study, researchers set out to determine the impact of psilocybin on the amygdala—a primitive part of the brain that helps process emotional reactions—as well as the compound’s effects on depression.
The study’s participants underwent fMRI brain scans prior to taking the drug.
The participants were then involved in two individual sessions, one week apart, in which they took doses of psilocybin prior to undergoing another fMRI the morning after consuming the second dose.
Science Alert went on to report:
During the fMRI scans, the group were shown images of faces with either fearful, happy, or neutral expressions, and the researchers wanted to investigate what effect these faces had on the participants’ amygdala after taking psilocybin.
After the experiment, the majority of patients reported that the psilocybin had eased their depressive symptoms, with almost half the group still seeing benefits from the treatment five weeks later – in line with the kinds of benefits other depression studies using the drug have shown.
More intriguingly, the fMRI scans showed the drug heightened activity in the right amygdala, with increased responses to both fearful and happy faces – and the increases to fearful faces were predictive of clinical improvements in depressive symptoms one week after the experiment.
“The major caveats are a lack of control group, a lack of SSRI group, and that the time point of investigation is only one day after the psilocybin session and not more than that. All of these caveats will be addressed in our next trial,”Roseman told PsyPost.
Revealing a major problem with the current pharmaceutical treatments model for depression, which attempts to negate emotional receptivity using SSRIs—the alleviation of depression using psilocybin is achieved by increasing emotional receptivity.
“It is important to emphasize that psilocybin-assisted therapy is a model in which the patient is undergoing a deep psychological process in one or few psychedelic sessions, in which he might have an intense cathartic experience, or peak experience,” Roseman explained.
A dose of psilocybin was administered in a controlled setting while professionals are on hand to provide the patients with psychological support. Typically, the patients receive counseling before and after each session, in an effort to assist them in preparing for, and integrating, their psychedelic experience.
“This is unlike antidepressants which are given as chronic pharmacological intervention with less psychological insights,” Roseman noted.
It is important to note that the study clearly shows that increased emotional receptivity being enhanced alleviates depression—almost the exact opposite of how SSRI antidepressants operate.
For full references please use source link below.