How a virus can save your life
Story at-a-glance
- Not all viruses are harmful to humans; some are natural bacterial predators and scientists are learning how to harness them to treat antibiotic resistant bacterial infections that have a high rate of mortality
- Interest in viral therapy was brought to the forefront after a researcher fought an antibiotic resistant acinetobacter infection with a bacteriophage and the patient, who was also her husband, fully recovered
- Cambridge University has re-estimated the number of deaths attributed to antibiotic resistant bacteria, increasing the number from 23,000 each year to 90,000
- An overly hygienic environment may reduce your natural viral and bacterial biome and negatively affect your ability to fight infection; avoid antibacterial soaps and chemicals, and avoid using antibiotics unless necessary
Humans are in a new arms race against bacteria able to evolve resistance to antibiotics at much faster rates than scientists can develop drugs.1 Antibiotic resistance and multidrug resistance have been driven by number of factors triggered by modern life.
Although overuse of antibiotics in humans is one factor, it's only one piece of the puzzle. In 2017, the U.S. Food and Drug Administration (FDA) officially banned antibiotic use on confined animal feeding operations (CAFOs) for the purpose of growth promotion. Antibiotic use now requires veterinary prescription.
However, antibiotics are dispensed as usual for the purpose of “disease prevention;” 80 percent of all antibiotics sold in the U.S. are used in industrial agriculture, with industry veterinarians continuing to support routine use.2
Another driving factor may be the particularly wide use of the herbicides, glyphosate and dicamba. Data reveal agrichemicals and antibiotics in combination increase the evolution of resistance. In fact, bacteria may develop antibiotic resistance thousands of times faster after they are exposed to particular herbicides in the environment.3
Field research suggests herbicides enhance the ability of bacteria to become antibiotic resistant and the resistance may be acquired at rates much faster than those predicted under laboratory conditions.4 More than statistics and information, multidrug resistance may be responsible for more than 90,000 deaths in the U.S. every year.5
Multidrug Resistant Organisms May Cause Over 90,000 Deaths Each Year
Since the 1940s,6 antibiotics have been used to treat infectious diseases caused by bacteria. The first released was penicillin. This and others greatly reduced the illness and death from conditions like pneumonia. However, today there are a number of antibiotic resistant bacteria, making treatment less effective and increasing the risk of death.
Although some bacteria are naturally resistant, most gain resistance through genetic mutation. These bacteria are called superbugs and may signal the end of effectiveness of antibiotic treatment. Each year, at least 2 million Americans are infected with antibiotic-resistant bacteria and past statistics suggested at least 23,000 people died as a direct result.7
Many more die from complications of an antibiotic resistant infection. However, a re-estimation of these deaths by Cambridge University now puts the number of annual deaths from drug-resistant infections closer to 90,000.8
Some of the more common antibiotic resistant bacteria are methicillin-resistant Staphylococcus aureus (MRSA), Streptococcus pneumoniae, carbapenem-resistant Enterobacteriaceae9 and Clostridium difficile.10 Each of these bacteria is capable of wreaking havoc on your health and potentially causing death.
A typical real-life example would be someone who has undergone a surgical procedure and contracts an infection. What should have been routine can now lead to a life-threatening struggle and medical emergency. However, this is not always the case, as infectious disease epidemiologist Steffanie Strathdee and her husband can attest.11
Viral Therapy Saved Researcher's Life
Evolutionary psychologist Tom Patterson and his wife Stephanie Strathdee were spending a week exploring pyramids and tombs in Egypt when Patterson experienced what appeared to be a bout of food poisoning. However, his condition rapidly deteriorated.
He was first flown to Germany and then to UC San Diego, where both he and his wife were on staff. Imaging and blood tests revealed a soccer-ball-sized cyst in his abdomen crawling with Acinetobacter, one of the most dangerous antibiotic-resistant bacteria.
Rarely found outside of the health care setting, the bacteria can trigger infections ranging from pneumonia to serious blood or wound infections.12 More frequently, this bacterium affects those with a weakened immune system, diabetes or chronic lung diseases.
The end of the antibiotic era has been described as an "unwinnable war" and the genus Acinetobacter epitomizes this trend as it displays mechanisms of resistance to all existing antibiotic classes.13 It was against this bacteria Strathdee began her crusade to save her husband's life.
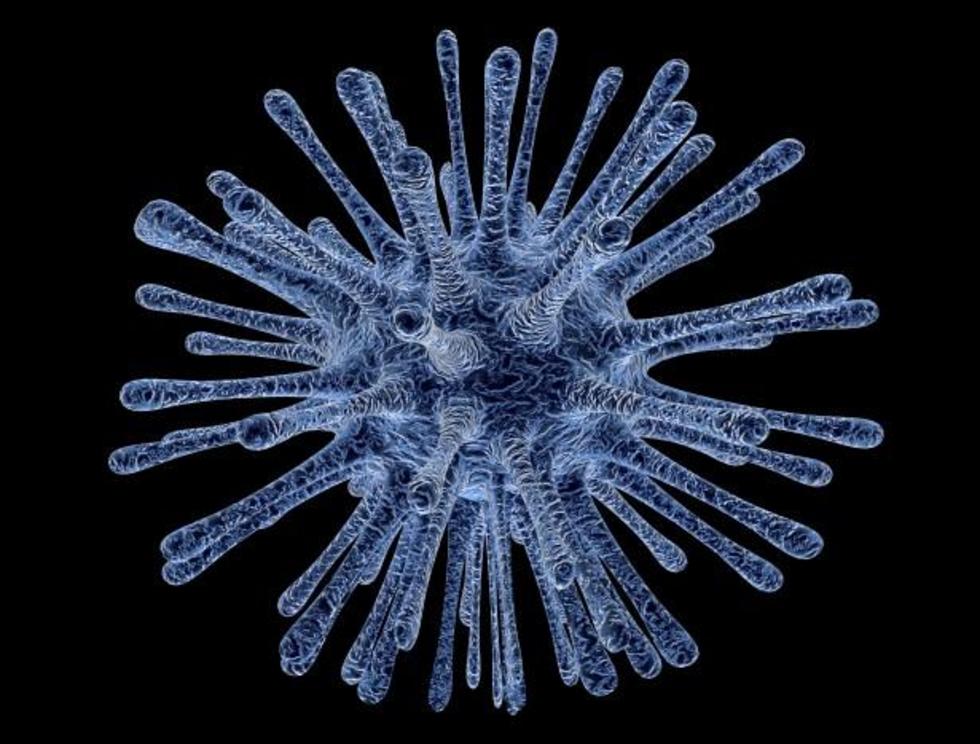
She first found a centuries-old Soviet bacteriophage cure while searching through PubMed for biomedical journal articles on treating superbugs.14 A bacteriophage refers to a virus that acts as a parasite; it infects the bacteria and reproduces inside it, devouring it in the process.
It was one of several alternative therapies she found for treatment. Strathdee worked with Texas A&M University and the U.S. Naval Medical Defense Command to obtain three bacteriophages able to strike Acinetobacter.
Patterson didn't learn of the treatment methodology until he came out of the coma in which he had been for two months.15 The pair describe their experience as different from most as they were given resources and had connections many don't have. That position of privilege allowed them to tell a positive story at the end of a nightmare.
Strathdee described the process of convincing Patterson's doctors to try this approach as going up against a risk-averse, litigious health care community that worries if an experimental treatment is tried and the patient dies, the physician will be sued.16 In this case, Patterson was at a teaching and research hospital where it was acknowledged he would die unless something drastic was initiated.
Some Viruses Are Natural Bacterial Predators
First written by the ancient Indian philosopher Kautilya in his classic treatise on economics and political science, "The Arthashastra,"17 "the enemy of my enemy is my friend," may have deep significance in the treatment of multidrug-resistant bacteria. While the political implications may have waned in a global economy,18 friendly viruses fighting harmful bacteria may become our best friends.
Also called viral therapy, this is the essence of bacteriophage treatment in which specific viruses are used to fight and kill harmful bacteria. Strathdee is currently conducting two clinical trials on it, one for individuals with ventricular assist devices who are infected with biofilm forming bacteria, and the other for patients with cystic fibrosis who develop antibiotic-resistant infections.
In patients with ventricular assistive devices, the phase I/II clinical trial will test the safety, tolerability and efficacy of bacteriophage therapy at UC San Diego and other teaching hospitals across the U.S. This multi-institution effort is the direct result of Patterson's treatment.19
Bacteriophages, also known simply as phages, are actually the most populous organisms on the planet20 targeting specific bacteria, and have been used for the last 90 years as a means of treating bacterial infections. Essentially, bacteriophages are viruses that infect bacteria and are harmless to humans.
How Phages Control Bacterial Growth
Although historically used, the process is only now being studied. In order to infect the bacteria, most phages have a tail that pierces the bacterium's membrane and inserts viral genetic material.21
Antibiotics work by affecting bacterial cell walls or the cells' protein building machinery, while bacteriophages exploit the bacteria and ultimately destroy it by infecting the cell and replicating itself, causing the bacteria to burst. This releases additional bacteriophages to kill neighboring bacteria.22
A typical cycle takes 30 to 60 minutes and stops when the pathogenic bacteria are eliminated, leaving nothing for the bacteriophage to infect. Bacteriophages are effective against biofilms, layers of aggregated bacteria and other extracellular components protecting the bacteria's cell walls from antibiotics.23
These bacteria form complex communities that may require very high concentrations of antibiotics, and often render infections very difficult to treat. By contrast, some bacteriophages are able to breach the shield and replicate locally, exposing the remaining bacteria to additional bacteriophages and the patient's immune system.
Bacteriophage therapies also have very few reported serious side effects, while all antibiotics have side effects. In combination with bacteriophage therapy, antibiotics may be effective at lower doses.24
Geopolitical Influence Slows Progress
Bacteriophages were discovered nearly simultaneously by Frederick Twort and Félix d'Hérelle. According to Strathdee's literature search,25 d'Hérelle had a difficult personality and tended to anger the medical and science community. Because he had no formal training, some worked to bury his findings.
The bacteriophage therapy was also vigorously used by the former Soviet Union, the Republic of Georgia and Poland, as it was discovered before modern-day antibiotics. By the fall of the Soviet Union, the Golden Age of phage-based therapy was over, with just a few labs continuing the work.26
Since access to penicillin in the Soviet Union was unreliable, Stalin and others embraced bacteriophage therapy to treat infections. As Strathdee describes, at that time, if you supported bacteriophage therapy in the U.S. you were labeled a communist.27
In the early years, bacteriophage therapy was used to treat dysentery and cholera. In one study,28 only 37 percent of untreated individuals suffering from cholera lived, while 92 percent of those treated with bacteriophages survived. With the exception of a few countries, bacteriophage therapy had been abandoned, as a treatment with antibiotics worked exceptionally well — until the last decade.
Bacteriophages are also more difficult to prepare29 as they must be isolated and then grown cleanly. Many of the early commercial products were of poor quality and led to the therapy being discredited.
Since one type of phage can infect only a few species of bacteria, selection has to be meticulously done. The process may take more time than a patient has, especially if they're used as a last resort on ill patients.30
Avoid Being Overly Hygienic
Children raised in an extreme hygienic environment, devoid of dirt and germs, are not able to build up a natural resistance to disease, making them more vulnerable later in life. This theory, known as the hygiene hypothesis, is likely one of the major reasons why allergies and immune system diseases have grown rapidly in the last several decades.
While the hygiene hypothesis simply states that exposure to multiple organisms will bolster your immune system, science is finding the reality is a bit more complex.31,32 However, trying to keep your environment overly sterile may indeed backfire and actually increase your risk of developing acute and chronic illnesses.
Exposure to a variety of microorganisms is one key to developing a strong immune system and a mucus substrate for a symbiotic relationship between beneficial viruses and bacteria. You can avoid being "too clean" and bolster your body's natural defenses by:
- Educating yourself on the differences between natural and artificial immunity, and making informed decisions about the use of vaccinations.
- Avoiding unnecessary antibiotics. Remember, viral infections are impervious to antibiotics, which only work on bacterial infections.
- Letting your child get dirty. Allow your kids to play outside in the dirt (and realize if your kid eats boogers, the world won't end).
- Avoiding antibacterial soaps and other antibacterial household products as these destroy the microorganisms your body needs exposure to for proper immune function. Simple soap and water are all you need for effective hand-washing. Antibacterial chemicals such as triclosan — which is now banned in hand soaps in the U.S. — are quite toxic and have been found to promote the growth of resistant bacteria and superbugs.
- Consuming organic, grass fed meats grown without antibiotics.